Morning Rounds
The Case of the Shimmering Spot
By Klaus Freeland, MD, and Eugene A. Milder, MD
Edited by Steven J. Gedde, MD
Download PDF
Laurie Mable* came to our urgent care eye clinic complaining of a spot in the vision of her left eye. The 63-year-old music teacher had noted the change just the day before and described it as a dull gray shimmering area just to the temporal side of her central vision, with rare photopsias. Ms. Mable was experiencing no pain, her vision was otherwise normal, and she was in what she described as her usual state of health. She denied having any recent viral or flu-like illnesses but had received her influenza vaccine 13 days prior to the onset of symptoms.
We Get a Look
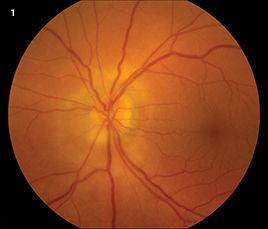
Ms. Mable’s visual acuity was 20/20 in both eyes and no afferent pupillary defect was detected at this time. The anterior chamber of her left eye was quiet, the cornea was clear, and there was mild nuclear sclerosis. In addition, her left eye showed subtle yellow-white peripapillary changes, deep to the retina, with patchy overlying retinal edema (Fig. 1). The funduscopic examination of her right eye was normal except for a known choroidal nevus. No vitritis was present in either eye.
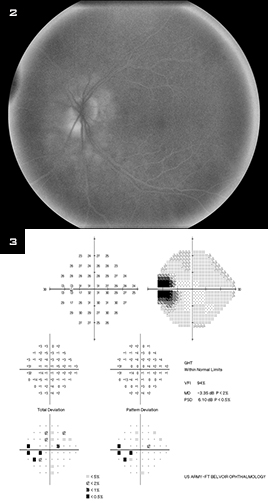
We examined her left eye further with fluorescein angiography and spectral-domain OCT. The angiogram showed peripapillary hyperfluorescence with late optic disc staining (Fig. 2), and the OCT confirmed the presence of peripapillary retinal edema.
In addition, Humphrey 30-2 visual field testing showed an enlarged blind spot in the left eye (Fig. 3). The right eye had a full visual field.
We initiated an extensive work-up that included an MRI of the brain and orbits with gadolinium and a panel of laboratory tests looking for infectious, inflammatory, or infiltrative causes of optic neuritis or neuroretinitis. However, the MRI results were normal, as were the lab results. (The latter included a CBC with manual differential; the rapid plasmin reagin and angiotensin-converting enzyme tests; and tests for Bartonella antibodies, Lyme disease, toxoplasmosis, and tuberculosis.) In addition, her blood pressure was normal. No treatment was prescribed, and within one week, Ms. Mable’s visual symptoms had resolved.
After six weeks of close follow-up, Ms. Mable’s visual acuity remained 20/20, and her visual field loss stabilized both subjectively and on repeat testing. The peripapillary edema resolved and a 1+ afferent pupillary defect was apparent. We concluded that this clinical scenario was most suggestive of acute idiopathic blind spot enlargement (AIBSE).
|
What's Your Diagnosis?
|
 |
|
The left eye showed subtle yellow-white peripapillary changes and patchy overlying retinal edema.
|
Background
AIBSE is a controversial diagnosis despite a slowly growing body of cases.1 In 1988, Fletcher et al. described blind spot enlargement in seven patients who did not have choroiditis or disc edema.2 It was unclear what the relationship was between these patients and those with multiple evanescent white dot syndrome (MEWDS) or if this represented a different manifestation of the same disease.
In 2001, a case series provided a better classification of AIBSE.1 There were 27 patients in the series, all of whom were women between the ages of 19 and 53. All had enlarged blind spots on automated perimetry. Twenty-five of the 27 patients complained of decreased vision. Visual acuity was normal in 16 of the patients and 20/50 or better in all but one of the patients. Nine of the 27 had dyschromatopsia, and eight had afferent pupillary defects. The most common findings included mild disc swelling or hyperemia and peripapillary subretinal pigmentary changes. Three of the patients had vitreous inflammation. Late staining of the optic nerve head and peripapillary area was common, and all patients with long-term follow-up had persistent visual field defects.1
 |
|
ADDITIONAL CLUES. (2) Peripapillary hyperfluorescence with late optic disc staining was evident on fluorescein angiography; and (3) visual field testing showed an enlarged blind spot in the left eye.
|
A New Mystery
Although Ms. Mable was slightly older than the patients in the published case reports, her visual symptoms fit the description of AIBSE. We were also intrigued by the timing of her symptoms, in that their onset followed closely upon her vaccination for influenza. In 1984, when Jampol et al. first described MEWDS, they pointed to the frequent history of a viral prodrome.3 There are also a few case reports of MEWDS occurring after vaccination for human papillomavirus, hepatitis A, and hepatitis B, but none after influenza vaccination.
With such striking similarities between MEWDS and AIBSE, it seems plausible that a postvaccination case of AIBSE could occur. Reports of additional cases of postvaccination MEWDS and AIBSE are needed to confirm this possible relationship.
___________________________
* The patient’s name is fictitious.
___________________________
1 Volpe NJ et al. Arch Ophthalmol. 2001;119(1):59-63.
2 Fletcher WA et al. Arch Ophthalmol. 1988;106(1):44-49.
3 Jampol LM et al. Arch Ophthalmol. 1984;102(5):671-674.
___________________________
Capt. Freeland is an ophthalmology resident at Walter Reed National Military Medical Center in Bethesda, Md., and at Fort Belvoir Community Hospital in Fort Belvoir, Va. Lt. Cmdr. Milder is a staff retina specialist and assistant chief of the ophthalmology service for the U.S. Navy at Fort Belvoir Community Hospital. The authors have no related financial interests.
___________________________
NOTE: The views expressed in this article are those of the author(s) and do not necessarily reflect the official policy or position of the U.S. Departments of the Navy, Army, or Air Force; the U.S. Department of Defense; or the U.S. government.
Calling All Cases!
Interested in sharing a case?
Submit it to us at:
Morning Rounds
EyeNet Magazine
655 Beach Street
San Francisco, CA 94109
Phone: 866-561-8558
or 415-561-8500
eyenet@aao.org
|