By Lauren Jeang, Priya Shah, MD, Patricia Chévez-Barrios, MD, and Rahul T. Pandit, MD
Edited by Steven J. Gedde, MD
Download PDF
Jane Smith* came to our clinic complaining of a one-week history of redness, tearing, and irritation in both eyes. The 68-year-old retired teacher told us that she had a long history of dry eyes and blepharitis that had been previously treated at a community clinic. In addition, Ms. Smith’s medical history was significant for seasonal allergies and breast cancer. Her cancer had been treated with a bilateral mastectomy, and she had received no chemotherapy or radiation. She was allergic to several fragrances and iodine, which gave her hives, and she used Visine eyedrops and loratadine (Claritin) as needed for her allergies.
We Get a Look
When we saw Ms. Smith, the external examination revealed rosacea. The slit-lamp exam showed normal conjunctivae, meibomian gland disease without collarettes, and punctate corneal epitheliopathy.
We diagnosed posterior blepharitis and secondary dry eye syndrome and started her on daily lid compresses, topical azithromycin 1 percent once a day, loteprednol 0.2 percent twice a day, and artificial tears.
Ms. Smith returned 20 days later with worsening ocular redness, lid crusting, and itching. She had discontinued her drops, thinking that she was allergic to one of them. The exam at this time revealed 1+ bulbar conjunctival injection and 2+ conjunctival follicles on both lower lids. We presumed that she was allergic to the azithromycin and resumed loteprednol at a higher dose of four times a day with a taper.
Ms. Smith returned three weeks later. Her symptoms had worsened, and our exam found increased 2+ conjunctival injection and 4+ lower lid follicular reaction.
Pinning It Down
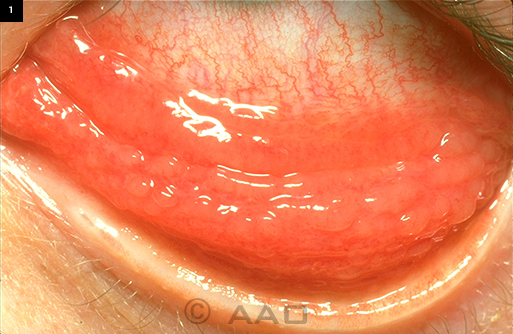
Ms. Smith’s presentation and examination results were consistent with chronic follicular conjunctivitis (Fig. 1). Our differential diagnosis included hypersensitivity reactions, such as medication side effects and allergic/ irritant hypersensitivities; infectious etiologies, including Chlamydia trachomatis and molluscum contagiosum; general inflammatory conditions, such as ocular rosacea; and conjunctival lymphoma.
Ms. Smith reported that she had accidentally used a fragrance the day before she saw us—and that, in the past, the fragrance had triggered a severe allergic reaction. We believed that she had a hypersensitivity response and recommended that she discontinue all drops, fragrances, and facial products.
At the next follow-up visit, her follicular reaction had worsened, although her bulbar injection had improved. We started difluprednate twice a day for both eyes and sent a Chlamydia culture, which returned negative. We also recommended a conjunctival biopsy as well as a dermatology consultation to evaluate for potential hypersensitivities, but Ms. Smith declined at this time.
With difluprednate treatment, Ms. Smith’s condition improved dramatically. However, when we tapered the difluprednate to loteprednol 0.5 percent, her follicular conjunctivitis returned. We suspected an allergy to loteprednol, so we restarted difluprednate with caution against its long-term use. Coincidentally, Ms. Smith’s facial rosacea had become much worse; as a result, she agreed to consult a dermatologist who specializes in contact dermatitis.
|
What's Your Diagnosis?
|
 |
|
Masquerade. The patient was initially diagnosed with follicular conjunctivitis, similar to the case presented in this image.
|
From Dermatology to Biopsy
The dermatologist conducted patch testing, which revealed a possible reaction to balsam of Peru (a fragrance additive) and propylene glycol, which is present in the artificial tears product Systane, which Ms. Smith had begun using. She showed no reaction to azithromycin, but a possible reaction to loteprednol and certain other steroids was noted.
Ms. Smith was advised to avoid all steroid drops, Systane, and any fragrances; and hypoallergenic home and hygiene products were recommended.
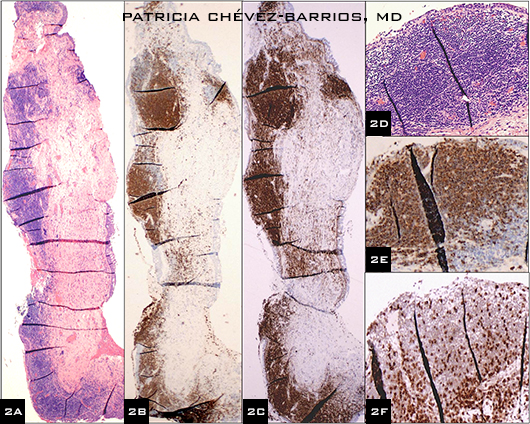
In addition, Ms. Smith agreed to a right palpebral conjunctival biopsy at this time. It revealed epithelium containing goblet cells and stroma with vaguely nodular lymphoid infiltrates associated with areas of fibrosis. The lymphocytic infiltrates did not form well-defined follicles.
The immunohistochemistry results (Fig. 2)—notably the elevated number of B cells with coexpression of BCL-2 and the infiltration of these cells into the epithelium—were consistent with low-grade mucosa-associated lymphoid tissue (MALT) lymphoma. A moleculase test did not reveal a monoclonal population. However, the tissue sample may have been insufficient, and the histopathology findings were enough for diagnosis.
 |
|
Histopathology results. This photo collage shows MALT lymphoma tis sue from the biopsy of the patient s right conjunctiva. (2A) Low power view of conjunctiva with nodular and diffuse infiltrate of lymphocytes (blue cells); hematoxylin eosin (HE) stain, 2× original magnification. (2B) Low power view note the predominant brown staining of the infiltrate; CD20 antibody stain and DAB chromogen, 2× original magnification. (2C) Coex pression of BCL 2 with CD20 (panel 2B), typical of B cell lymphomas; BCL 2 antibody stain and DAB chro mogen, 2× original magnification. (2D) High power view of the subepi thelial lymphoid infiltrate, which was composed of small lymphocytes with out true lymphoid follicle formation; HE stain, 20× original magnification. (2E) High power view of the lym phoid infiltrate seen in 2D but with CD20 immunostain for B cells labeling the majority of the cells; CD20 anti body stain and DAB chromogen, 20× original magnification. (2F) The same area as seen in 2D and 2E but with CD3 immunostain for T cells note the scant number of T cells as com pared with the number of B cells; CD3 antibody stain and DAB chromogen, 20× original magnification.
|
Discussion
Ocular adnexal lymphoma (OAL) includes lymphomas of the orbit and surrounding eye tissues. It is fairly common and comprises 11 percent of orbital masses and 34 percent of orbital malignancies.1 Roughly 60 to 86 percent of OAL cases are unilateral and primary.1 These are most commonly MALT-type follicular and small lymphocytic lymphomas. In contrast, OAL that is bilateral and/or is accompanied by systemic involvement is often associated with more aggressive disease.1 Patients with primary OAL have a lower risk of recurrence and progression compared with those with bilateral or systemic disease.1
MALT lymphoma is the most common lymphoid neoplasm of the conjunctiva.2 It tends to appear in the fornix or bulbar conjunctiva as painless, sessile, and pink patches.2 The most common presenting symptoms are swelling or presence of a mass.3 However, as seen in Ms. Smith’s case, conjunctival lymphoma does not always appear with these characteristics. Instead, it may present with nonspecific symptoms (such as irritation, tearing, or blurry vision) that lead to a diagnosis of allergic or chronic conjunctivitis.2,3
Given the difficulty in diagnosis, physicians are encouraged to carefully examine for lesions by using significant eyelid eversion and eyeball movement.2 Once a diagnosis of conjunctival lymphoma is made, an orbital CT scan, a complete blood count with differential, liver function tests, and chest X-rays should be ordered.4
Treatment and Prognosis
Patients with MALT lymphoma respond well to radiation therapy.3,4 Despite the indolent disease course, there may be recurrences, which usually can be controlled with therapy. Patients have a good 10-year survival rate.1,3,4 Some studies suggest that primary therapy with rituximab may be effective, but its benefits over radiation therapy have not been determined.1
Back to Our Patient
Ms. Smith received orbital radiation—24 gray (Gy) in 16 fractions at 1.5 Gy/fraction dose—and has done well without experiencing any local side effects. To date, she has no signs of systemic disease. Although OAL is relatively common, her case serves as a reminder that OAL may not always be typical, and a systematic method of ruling out possible causes of chronic follicular conjunctivitis remains essential.
___________________________
* Patient’s name is fictitious.
___________________________
1 Rootman DB et al. Ophthal Plast Reconstr Surg. 2011;27(6):405-409.
2 Hata M et al. Clin Ophthalmol. 2013;7:663-666.
3 Fung CY et al. Int J Radiat Oncol Biol Phys. 2003;57(5):1382-1391.
4. Suh CO et al. Int J Radiat Oncol Biol Phys. 2006;65(1):228-233.
___________________________
Ms. Jeang is a fourth-year medical student, and Dr. Shah is a medical researcher; both are at Baylor College of Medicine in Houston. Dr. Chévez-Barrios is professor of pathology and laboratory medicine and ophthalmology and Dr. Pandit is assistant professor of ophthalmology; both are at Weill Cornell Medical College at Houston Methodist Hospital. The authors report no related financial interests.