By Valentina P. Lozano, MD, Matthew J. Gray, MD, Ahmad Alkhasawneh, MD, and Anup Kubal, MD
Edited by Steven J. Gedde, MD
Download PDF
Heidi Goldberg* would never let anything stop her from going on her annual summer trip to Europe with her husband. Despite developing blurry vision, intermittent photophobia, and right conjunctival injection before her departure, this 61-year-old Caucasian woman decided to postpone seeing the doctor until after she had returned from vacation.
We Get a Look
By the time we saw Ms. Goldberg in November 2013, it had already been four months since her ocular symptoms began.
An outside ophthalmologist, who saw her a week prior to this visit, noted an intraocular pressure (IOP) of 32 mmHg in the right eye and 11 mmHg in the left eye. That ophthalmologist had diagnosed Ms. Goldberg with anterior uveitis with ocular hypertension in the right eye and prescribed dorzolamide drops twice a day and topical prednisolone four times a day. After five days of treatment, Ms. Goldberg had no symptomatic improvements.
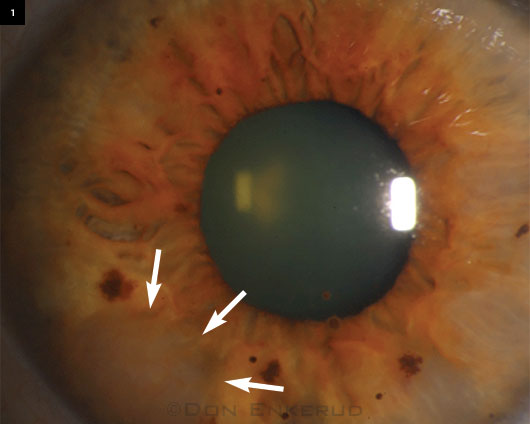
On our exam, her visual acuity was 20/20 in both eyes. IOP was 21 mmHg in her right eye and 14 mmHg in her left. Slit-lamp examination of the right eye showed conjunctival injection and keratic precipitates. The anterior chamber was deep and had 3+ cell with trace flare. Interestingly, we noted that the right iris showed multiple diffuse, elevated nodular infiltrates with increased vascularity extending to the angle nasally and inferiorly, as well as inferotemporally (Fig. 1).
Fundus examination of both eyes was normal.
Her Medical History
Ms. Goldberg’s medical history included hypothyroidism and shingles on the right side of her face with ocular sparing.
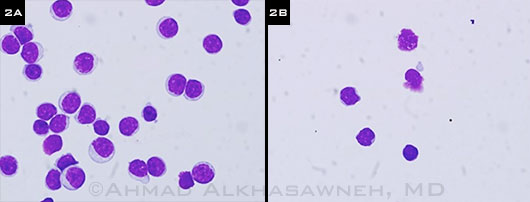
In 2003, she was incidentally diagnosed with chronic lymphocytic leukemia (CLL), which was discovered through routine blood work and subsequent cell flow cytometry. For 10 years after her diagnosis of CLL, she remained asymptomatic despite having severe thrombocytopenia, for which she refused treatment. In February 2013, she developed splenomegaly and easy bruising, which prompted her oncologist to proceed with a bone marrow biopsy. This revealed 100 percent cellularity of marrow and 90 percent CLL involvement (Fig. 2A). Due to a persistent platelet count below 40,000 and new onset of symptoms, she received four weekly intravenous infusions of rituximab 375 mg/m2, but there was no improvement in her platelet count.
 |
|
AT THE SLIT LAMP. When we first saw the patient, we noted diffuse nodular infiltrates in the iris.
|
The Differential Diagnosis
Ms. Goldberg’s history gave us much to consider. The differential diagnosis for her anterior uveitis at that point included ocular malignancy, autoimmune disease, and infection (classically tuberculosis, syphilis, and Lyme disease).
Although leukemic infiltration of the iris was the highest on our differential, we were unable to rule out an iris melanoma or a secondary metastatic process. Although a biopsy was indicated to help determine the diagnosis, it was delayed due to her persistently low platelet count. Her treating hematologist recommended preoperative chemotherapy to increase her platelet count. This was ineffective and the decision was made to proceed with the biopsy despite her persistent thrombocytopenia.
Additionally, we ordered a routine autoimmune and infectious workup for iritis, including the following tests: ANA (antinuclear antibodies), ANCA (antineutrophil cytoplasmic antibody), ACE (angiotensin-converting enzyme), RPR (rapid plasma reagin), PPD (purified protein derivative), and Lyme disease. The results were negative.
A fine-needle aspiration of the right iris was done, using the technique described by Shields et al.1 to avoid seeding surrounding tissue with malignant cells. Although an anterior chamber paracentesis was initially considered, a biopsy was felt to be the better option, given our broad differential and desire to avoid multiple invasive procedures. She tolerated the procedure well, with minimal intraocular bleeding; and on postoperative day one, there were no signs of hyphema or any other complications.
Cell flow cytometry of the specimen revealed neoplastic lymphocytes with clumped chromatin and scanty cytoplasm consistent with CLL (Fig. 2B).
 |
|
BIOPSIES. (2A) Nine months before we saw Ms. Goldberg, a bone marrow smear (cytospin) revealed neoplastic lymphocytes with clumped chromatin and scanty cytoplasm. (2B) We ordered a biopsy of the iris (cytospin) that revealed leukemic cells with similar morphology to bone marrow lymphoma (Giemsa stain, 100×).
|
Discussion
A PubMed search of anterior uveitis and chronic lymphocytic leukemia yielded only 10 results.2-11 These 10 studies described cases of anterior uveitis caused by leukemic infiltrates in patients with CLL. Six of these cases had been previously diagnosed with CLL, and four were diagnosed based on ocular pathology as their presenting abnormalities. The cases were similar to Ms. Goldberg’s in that they presented with several weeks of blurry vision, eye redness, eye pain, and photophobia, and were refractory to topical steroids. In most cases, the fundus exam was normal.
Leukemic infiltrates in the eye usually occur in well-vascularized areas of the posterior segment, such as the retina and choroid. Leukemia rarely presents with anterior uveitis, especially when the type of leukemia is chronic.12
In the 10 cases that we reviewed, the authors reported that making the diagnosis of anterior uveitis caused by CLL infiltration was challenging, and most cases required a sample of tissue or ocular fluid to confirm the diagnosis. Treatment varied, with patients receiving either systemic chemotherapy or immunotherapy, local irradiation, or a combination of treatments.
Our patient was already on a regimen of systemic chemotherapy. After her diagnosis, she continued to receive treatment by her hematologist. On her seven-month follow-up, her ocular complaints had resolved and her exam had normalized.
Treatments and outcomes of the cases reported in the literature were very individualized; thus, it is difficult to make a generalization about the best treatment. Although our patient had a favorable outcome with systemic chemotherapy alone, we cannot conclude that this is the optimal treatment for all patients. Each patient must be assessed on an individual basis, and a treatment plan must be tailored to fit the patient’s and caregiver’s goals.
This case report also demonstrates the need to consider masquerade syndromes like CLL when evaluating patients with visual complaints of anterior uveitis that is refractory to topical steroid, regardless of malignancy history.
Be Published in EyeNet!
Morning Rounds. If you had a mysterious or challenging case, share it with your colleagues.
Ophthalmic Pearls. Review a medical condition or surgical procedure.
Blink. Got an image that is perplexing or intriguing? Let us showcase it.
Letters. EyeNet welcomes your correspondence on all ophthalmic issues.
How to get started. Visit “Write for Us.”
|
___________________________
* Patient name is fictitious.
___________________________
1 Shields CL et al. Ophthalmology. 2006;113(11):2080-2086.
2 Newman NM et al. Surv Ophthalmol. 1972;16(5):316-321.
3 Burton BJ et al. Br J Ophthalmol. 2005;89(6):775-776.
4 Belmont J et al. Journal of Ocular Therapy & Surgery. 1985;4(4):125-129.
5 Martin B. Br J Ophthalmol. 1968;52(10):781-785.
6 Glaser B, Smith JL. Br J Ophthalmol. 1966;50(2):92-94.
7 Mohsenin A et al. Clin Ophthalmol. 2012;6:2045-2047.
8 Gupta G et al. Retina. 2007;27(9):1311-1312.
9 Kubicka-Trzaska A et al. Klin Oczna. 2010;112(10-12):314-317.
10 Grishko NI, Sudenko VM. Oftalmol Zh. 1966;21(5):390-391.
11 Bronner A et al. Bull Soc Ophtalmol Fr. 1976;76(2):201-204.
12 Allen RA, Straatsma BR. Arch Ophthalmol. 1961;66(4):490-508.
___________________________
Dr. Lozano starts an ophthalmology residency this year at the University of Florida. Drs. Gray and Kubal are both assistant professors of cornea and external diseases, and Dr. Alkhasawneh is a hemopathology fellow; all three are at the University of Florida in Gainesville. The authors report no related financial interests.
___________________________
Acknowledgements: The authors would like to thank Jay Lynch, MD, and Gabriela Fernandez, MD, for reviewing their article thoroughly.