By Wan Wan Xu, MD, and Robert S. Feder, MD
Edited by Steven J. Gedde, MD
Download PDF
Stella Grundy* came to see us for a cataract evaluation. She was a 40-year-old woman who had started to notice gradually worsening foggy vision in her left eye. She reported that she had undergone cataract surgery in her right eye five years ago and was happy with the result. She also had previously been diagnosed with retinitis pigmentosa.
The Eye Exam
In her left eye, visual acuity was 20/70 with no improvement on pinhole. Her manifest refraction was –8.75 sphere. Her intraocular pressure (IOP) was 10 mmHg.
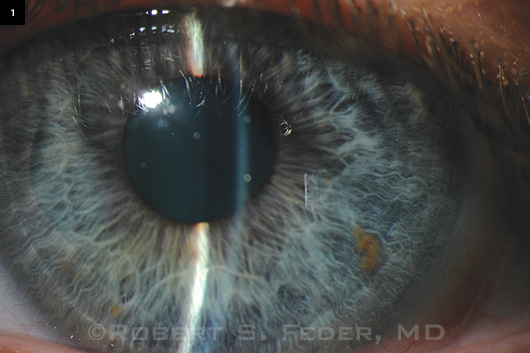
On slit-lamp biomicroscopy, she had a shallow anterior chamber and 2+ posterior subcapsular cataract, with no evidence of nuclear cataract (Fig. 1). Fundus exam showed bilateral disc pallor, arteriolar narrowing, and pigmentary changes with no staphyloma or other fundus findings seen in high myopia. The fundus exam was consistent with her long-standing diagnosis of retinitis pigmentosa.
A Power Puzzlement
Because she was highly myopic in her left eye, we expected to place a lens with a power of around 12 D. However, her IOLMaster printout recommended a ZCB00 lens (Abbott Medical Optics) of 21 D with residual power of 0.06 D using the SRK/T formula. Her expected and resultant IOL power were drastically different, and we had to figure out why.
First, we looked at her biometric data. An A-scan axial length showed that the eye was 22.8 mm long, which would be expected to predispose her to slight hyperopia, not high myopia. Corneal topography showed that her central pachymetry was 483 µm.
Her flat K was 44.4 D, and steep K was 47.4 D, with 3 D of astigmatism at 87 degrees. Belin/Ambrosio analysis did not show any signs of ectasia. Because Ms. Grundy’s keratometry readings were not markedly steep, they were not sufficient to explain her manifest refraction.
Once we had determined that the extra power was not due to axial length, corneal curvature, or staphyloma, we then considered the lens.
To get a better view of the anterior chamber in cross section, we obtained Scheimpflug images. They showed that the anteroposterior (AP) diameter of her lens was longer than usual (Fig. 2), measuring 5.5 mm. In comparison, an age-matched myope had a corresponding measurement of 4.3 mm.
Based on her eye measurements and Scheimpflug images, we made a diagnosis of spherophakia.
 |
|
WHAT'S YOUR DIAGNOSIS? (1) At the slit lamp, we note a shallow anterior chamber.
|
The Surgery
Ms. Grundy’s surgery was notable for several reasons.
First, the capsulorrhexis was difficult because of the shallow anterior chamber.
And during hydrodissection, it became clear that her lens was spherical, and nudging the lens in the bag caused it to tumble easily onto its side.
In addition, we extracted more lens material than would be expected in a typical phacoemulsification.
Moreover, an area of zonular dehiscence was noted, and we placed a capsular tension ring. An SN6AT7 21.5 D lens (Alcon) was inserted. Ms. Grundy’s postop refraction was –50 + 0.50 × 180.
Her pseudophakic right eye had similar measurements and postop refraction.
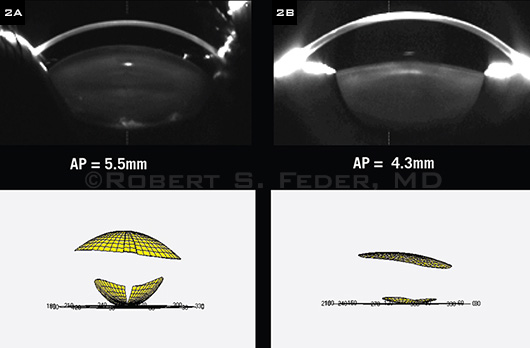 |
WE GET A CLOSER LOOK AT THE ANTERIOR CHAMBER. (2A) Our patient’s Pentacam Scheimpflug image and volumetric rendering of anterior and posterior surfaces of the lens. (2B) Corresponding images from an age-matched myope.
|
Discussion
Spherophakia is a condition in which the crystalline lens assumes a spherical shape with an increased AP diameter and a reduced equatorial diameter. The mean sagittal lenticular diameter for normal lenses has been reported as 4.3 to 4.6 mm.1,2 whereas Ms. Grundy’s AP diameter was 5.5 mm.
Spherophakia is most commonly seen in Weill-Marchesani syndrome, a rare connective tissue disorder that is also characterized by short stature, brachydactyly, and stiff joints. Spherophakia can also be associated with megalocornea, metaphyseal dysplasia, and sulfite oxidase deficiency. Patients with spherophakia are at risk for lenticular myopia, ectopia lentis, and angle-closure glaucoma.
Angle-closure glaucoma can occur in spherophakia through a pupillary block mechanism caused by dislocation of the lens into the anterior chamber or by forward movement of the lens. Pupillary block is exacerbated by miotics, which cause ciliary muscle contraction, loosen zonular support, and allow forward movement of the lens. It can be relieved by mydriatics, which relax the ciliary muscle, tighten zonular support, and cause posterior lens movement.
Our patient did not have the physical characteristics of Weill-Marchesani syndrome. However, she did have retinitis pigmentosa and an electroretinograph that was extinguished, consistent with a rod-cone dystrophy. We are investigating whether her spherophakia is linked to her retinitis pigmentosa.
___________________________
* Patient name is fictitious.
___________________________
1 Shufelt C et al; for the Los Angeles Latino Eye Study Group. Invest Ophthalmol Vis Sci. 2005;46(12):4450-4460.
2 Olsen T et al. Acta Ophthalmol Scand. 2007;85(4):361-366.
___________________________
Dr. Xu is a third-year ophthalmology resident and Dr. Feder is professor of ophthalmology and chief of the cornea service; both are at Northwestern University. Both authors report no related financial interests.