By David A. Plager, MD, with Fiona E. Costello, MD, and Sharon F. Freedman, MD
Download PDF
Optical coherence tomography (OCT) is well into its second decade of clinical use. As is typical of new technologies, it was initially tested, validated, and used in adults. Therefore, uncertainty exists about how best to apply it to children. Here, in part 1 of a 2-part series, David A. Plager, MD, of Indiana University and Riley Hospital for Children, hosts a discussion with Sharon F. Freedman, MD, of Duke University Eye Center, and Fiona E. Costello, MD, FRCPC, of the University of Calgary. The experts discuss their use of OCT in daily practice, including how they obtain and interpret OCT data for the pediatric population.
OCT in Pediatrics
Dr. Plager: A decade or so ago, most pediatric ophthalmologists did not use OCT routinely. How highly do you value OCT in your clinical practice today?
Dr. Freedman: I have a large pediatric glaucoma practice, and OCT has become indispensable to me. However, there are some patients for whom I can’t easily perform OCT, including very young children and those with a developmental delay.
Dr. Costello: As a neuro-ophthalmologist, I diagnose, manage, and treat a wide variety of optic nerve diseases. For me, OCT yields quantifiable structural metrics that I can compare with functional outcomes. I don’t interpret OCT findings in isolation, but I have found OCT to be an invaluable resource. I treat more adults than children in my practice, but I’m asked frequently by my pediatric neurology or ophthalmology colleagues to evaluate cases that may be papilledema or pseudopapilledema. OCT is useful in that context when combined with a thorough history and good functional metrics.
Longitudinal data, including OCT results and other measures of structural and functional integrity in the afferent visual pathway, are especially helpful. For instance, if I see big shifts in OCT measures of retinal nerve fiber layer (RNFL) thickness over time, I would consider true optic disc swelling as a possibility, rather than an anomalous disc. In a patient with optic neuritis, I might see elevated peripapillary RNFL measurements acutely, and then I’ll detect thinning of the peripapillary RNFL over time, often in concert with ganglion layer loss.
In general, I use OCT once I have developed a clinical hypothesis—for instance, if I suspect optic neuritis or mild papilledema. And the longitudinal changes in OCT findings will confirm or refute my hypothesis.
Advantages of OCT
Dr. Plager: What information does OCT provide that traditional tests, like visual fields or funduscopy, do not?
Dr. Costello: A longstanding notion is that two-thirds of adult patients and one-third of pediatric patients will have a normal-appearing optic nerve at the time of an acute optic neuritis event. In reality, because of axoplasmic flow stasis, most patients with optic neuritis have thickening of the peripapillary RNFL in their affected eye relative to the unaffected fellow eye. OCT affords a level of precision that cannot be achieved by qualitative assessment of the nerve. Traditional tests also are susceptible to interobserver disagreement, such as whether or not a nerve is swollen or pale.
OCT allows us to follow changes over time that may not be apparent by simple observation, such as subtle thickening of the RNFL in acute optic neuritis or gradual thinning of the RNFL that correlates with functional losses in low-contrast letter acuity testing or visual field testing in an evolving optic neuropathy. Quantifiable OCT measures of the neuroaxonal integrity of the afferent visual pathway can be correlated with outcomes, such as low-contrast or high-contrast letter acuity or visual field sensitivity. For adults as well as children, OCT allows me to understand the effect of an insult to the optic nerve, which is specific to the mechanism at hand, including ischemic optic neuropathy, post-papilledema optic atrophy, or inflammatory optic neuritis.
Structure Versus Function
Dr. Plager: How do structural results of OCT relate to functional results of a visual field or acuity test?
Dr. Costello: It depends on the disease process. In a clinically-overt optic neuritis event, a patient may sustain up to a 20% loss in peripapillary RNFL thickness, relative to the unaffected eye, yet maintain good functional outcomes by traditional metrics such as high-contrast visual acuity and standard automated perimetry.1 In cases of RNFL thickness loss exceeding 25%, the results of conventional testing (for example, mean deviation on standard automated perimetry) have been shown to correlate linearly with the extent of axonal loss, measured as the peripapillary RNFL thickness around the nerve.
Similarly, with other optic neuropathies, there are robust structural and functional relationships, but these relationships may not emerge until we reach a “tipping point” at which point the patient has too much axonal damage or neuronal loss to maintain normal function by conventional measures.
In idiopathic intracranial hypertension, the structural-functional correlation is low in the acute phase. Thickening of the RNFL correlates with more severe optic disc edema. However, good visual field function usually is maintained until damage is sustained to the optic nerve. With ensuing optic atrophy a relationship could emerge between visual function (assessed by standard automated perimetry or high-contrast visual acuity) and axonal integrity or neuronal loss (demonstrated by the thickness of the peripapillary RNFL or ganglion layer, respectively).
Normative Data
Dr. Plager: Based on existing normative pediatric data, can we be confident that results of a single OCT are normal or abnormal?
Dr. Freedman: The short answer is that we cannot. Dr. Mays El-Dairi and I, along with other investigators, have been involved in collecting normative OCT data for children,2,3 but pediatric normative values generally have not been incorporated into OCT analysis software.
There are large differences among ethnicities in normative OCT findings. For example, African American children and Caucasian children have different ranges of norms for optic nerve head size and refractive error. However, in our experience, the RNFLs of 3- to 18-year-olds generally are similar to those of the youngest cohort (age 18-24) represented in commercial OCT machines. Unfortunately, even adult normative values are incomplete, and most OCT machines have limited datasets. The original Spectralis OCT (Heidelberg Engineering) is constrained to a dataset from Caucasian adults, while a newer set includes multiple ethnicities.
Special attention should be given to the symmetry of findings. For example, if you see a little temporal thinning in a patient who has myopia with a tilted nerve, it’s not a major cause of concern if the abnormality is stable and symmetric between the eyes.
Dr. Costello: When I review OCT findings, I consider factors like intereye symmetry, optic disc area, and the morphological appearance of the optic nerve.
Longitudinal OCT data are crucial for detecting subtle changes. A nerve that is stable over time in an asymptomatic patient is highly reassuring. If ganglion layer measurements are normal longitudinally, that’s also reassuring because this layer is often the first to be lost in an acquired optic nerve injury in an adult. It’s important to emphasize that a piece of information gleaned from a single time point offers far less diagnostic utility than a constellation of findings attained over time.
Equipment Preferences
Dr. Plager: How machine-specific are the parameters measured by OCT?
Dr. Costello: When I was a fellow, we used mainly Zeiss technology: the Stratus OCT and then the Cirrus HD OCT (both by Carl Zeiss Meditec). In my practice environment, there was a lot of comfort with this technology. Now I use the Cirrus HD OCT and the (Heidelberg) Spectralis OCT together. I think that the technology has evolved, and both devices have advantages. The additional information afforded by head-to-head comparisons of OCT data from different machines can provide helpful insights. I have a relative scotoma for some of the other OCT models, so I can’t speak with expertise about the perks and pitfalls of these machines.
Dr. Freedman: I had some difficulty going from time-domain (TD)-OCT to spectral-domain (SD)-OCT, but I think there is consensus among practitioners that SD-OCT offers superior accuracy and precision, and it has become the mainstay of OCT technology. However, there are times when pediatric scans from these machines can have errors in segmentation of the RNFL and other retinal layers, requiring manual correction or at least the recognition that the quantitation of these respective layers is inaccurate.
I prefer the Spectralis for the pediatric population because it has an eye tracking feature, and the same machine will scan the patient the same way at each session. If a measurement around the optic nerve is a bit offset in the eye once, the machine will perform the scan the same way the next time.
I have found that as long as you perform all follow-up measurements of the same patient with the same OCT device, global metrics like the average RNFL will be remarkably similar for a stable case. If you are concerned only about global OCT measures, I think there is fairly good consistency between the Cirrus and the Spectralis instruments.
Dr. Costello: I think the key is to have good reliability criteria for the tool you’re using. Make sure the signal-to-noise ratio is good. Make sure you’re dealing with an experienced technologist and have a high-quality scan. Use the same scan, and don’t flip-flop between machines. For research purposes, it’s preferable to use the same machine that your colleagues use because you can’t conduct multicenter studies with competing technologies that have subtle differences.
Anesthesia-Related Pros and Cons
Dr. Plager: Because of young age or problems with cooperation, it can be very challenging to collect OCT data from pediatric patients. Is there a good way to perform OCT on a child who is under anesthesia?
Dr. Freedman: Yes, but it depends on the type of information you want. Detailed structural data can be obtained with the Bioptigen handheld device (now sold as Envisu, Leica). This device is especially useful for evaluating the macula or posterior pole, such as for macular dysfunction, epiretinal membrane, macular edema, or retinoschisis. I would recommend it for routine OCT in pediatric patients under anesthesia.
Obtaining RNFL measurements in anesthetized children has been very difficult. The Bioptigen handheld device lacks integrated software for quantitative analysis, so we have been trialing the Spectralis Flex (Spectralis on an adjustable arm on a movable stand). Scanning can be performed while the patient is supine. The OCT unit is mounted on the adjustable arm and can be positioned overhead, and although it is cumbersome to use, the Spectralis Flex can yield RNFL measurements. This approach may allow you to image a child with glaucoma and nystagmus who cannot cooperate in the seated position. Such a patient would require examination under anesthesia anyway, and with this instrument, you can actually do so. The IStand option of iVue (Optovue) also enables OCT under anesthesia, although I think the imaging quality is superior with the Bioptigen device. I expect that better technologies will emerge in the near future.
Dr. Costello: I agree with Dr. Freedman’s perspective.
More at the Meeting
Use the Academy Plus course pass to attend pediatric ophthalmology courses, such as the following:
Update on Diagnosis and Management of ROP (206). When: Sunday, Nov. 12, 10:15 a.m.-12:30 p.m. Where: Room 389.
Pediatric Eye Emergencies You Don’t Want to Miss! (243). When: Sunday, Nov 12, 2:00-3:00 p.m. Where: Room 386.
Principles of Pediatric Ocular Trauma Management (494). When: Monday, Nov. 13, 2:00-4:15 p.m. Where: Room 388.
Pediatric Ocular Tumors (550). When: Monday, Nov. 13, 4:30-5:30 p.m. Where: Room 238.
Concise Review in 2017: The Developmental Glaucomas (619). When: Tuesday, Nov. 14, 9:00-11:15 a.m. Where: Room 388.
What’s New and Important in Pediatric Ophthalmology and Strabismus for 2017 (644). When: Tuesday, Nov. 14, 10:15 a.m.-12:30 p.m. Where: Room 238.
|
Differentiating Papilledema From Pseudopapilledema
Dr. Plager: In the initial evaluation of a child referred for suspected papilledema, how helpful is OCT in differentiating optic nerve edema from pseudopapilledema—that is, buried drusen?
Dr. Costello: No practitioner needs to perform OCT to diagnose obvious optic disc drusen. If I see drusen littering the optic nerve on funduscopic examination, OCT testing would not add any diagnostic precision. Similarly, if I see prominent optic disc edema with peripapillary hemorrhage in a patient who’s symptomatic from manifestations of raised intracranial pressure, OCT findings are not needed for my diagnosis.
On the other hand, in the setting of a patient with very mild optic disc elevation, you do not want to miss raised intracranial pressure, but you also want to avoid unnecessary invasive testing. For a case like that, OCT is especially valuable.
Enhanced-depth imaging can be used to distinguish true optic nerve edema from pseudopapilledema. For instance, in buried disc drusen, a hypodense core and a hyperreflective margin may be observed.
I use OCT to look for longitudinal changes that are consistent with true papilledema versus a slightly anomalous disc (or pseudopapilledema with or without drusen). In cases of mild papilledema, there are often changes in the measured RNFL thickness that exceed the test-retest variability of the machine. Admittedly, I have been humbled by cases that appeared to involve just a slightly crowded nerve but actually represented mild papilledema due to raised intracranial pressure, which became evident over the course of follow-up.
Cases like these highlight the need for longitudinal follow-up, the importance of maintaining a high degree of suspicion, and the need to err on the side of caution. If you see a patient with presumed raised intracranial pressure, do the appropriate tests and neuroimaging and order a lumbar puncture. With newer enhanced-depth imaging, we may be able to spare patients with buried disc drusen from unnecessary invasive tests, but we still must use good clinical judgment.
Dr. Freedman: I agree. In fact, idiopathic intracranial hypertension can be accompanied by buried disc drusen, so drusen is not always a reassuring sign.
Dr. Costello: That is correct. Nevertheless, techniques in OCT are improving, and neuroradiologists have defined subtle magnetic resonance imaging findings that correlate with raised intracranial pressure. With an understanding of just how subtle the clinical symptoms could be—and by applying OCT with other tests—we won’t miss these cases.
___________________________
Listen to the roundtable below:
Download Audio
___________________________
1 Petzold A et al. Lancet Neurol. 2010;9(9):921-932.
2 El-Dairi M et al. Arch Ophthalmol. 2009;127(1):50-58.
3 Lee H et al. Invest Ophthalmol Vis Sci. 2016;57(9):OCT69-79.
___________________________
Dr. Costello is Associate Professor in the Departments of Surgery and Clinical Neurosciences at the University of Calgary. Relevant financial disclosures: None.
Dr. Freedman is Chief of Pediatric Ophthalmology and Professor of Ophthalmology and Pediatrics at Duke University Eye Center. Relevant financial disclosures: None.
Dr. Plager is Professor of Ophthalmology at Indiana University School of Medicine and a pediatric ophthalmologist at Riley Hospital for Children in Indianapolis. Relevant financial disclosures: None.
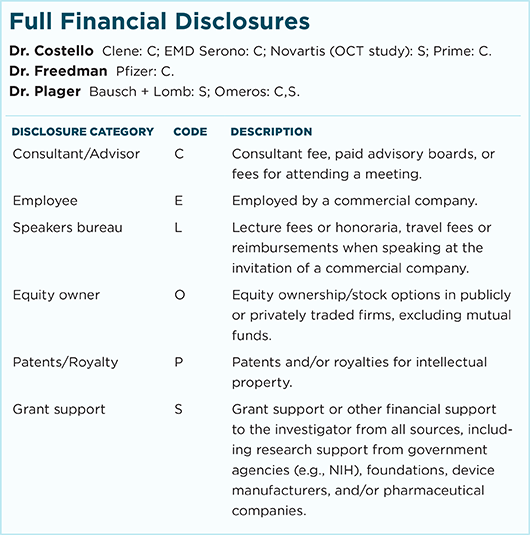
For full disclosures and the disclosure key, see below.