By Lori Baker-Schena, MBA, EdD, Contributing Writer, interviewing Jane C. Edmond, MD, Mays A. El-Dairi, MD, Mary Elizabeth Hartnett, MD, Ramiro S. Maldonado, MD, and J. Timothy Stout, MD, PhD, MBA
Download PDF
Optical coherence tomography (OCT) has proved to be a revolutionary retinal diagnostic imaging tool. Initially, however, it was not suitable for use in young children, as the tabletop design requires the patient to fixate on a target.
That all changed in 2008, when researchers at Duke University pioneered the use of a handheld spectral-domain (SD-OCT) system for examining infants with shaken baby syndrome.1 The introduction of this device, along with research on how to identify correct OCT settings in the pediatric population, has led to a recent surge of research on the developing retina.
“We were a little late getting on the OCT bandwagon,” acknowledged Jane C. Edmond, MD, at Baylor College of Medicine and the Texas Children’s Hospital. “The technology was first embraced by glaucoma and retina specialists, but its third utility—the ability to study the pediatric optic nerve—has become an important adjunctive tool.”
Here’s an overview of some potential applications of OCT in diagnosing and treating pediatric eye disease.
 |
|
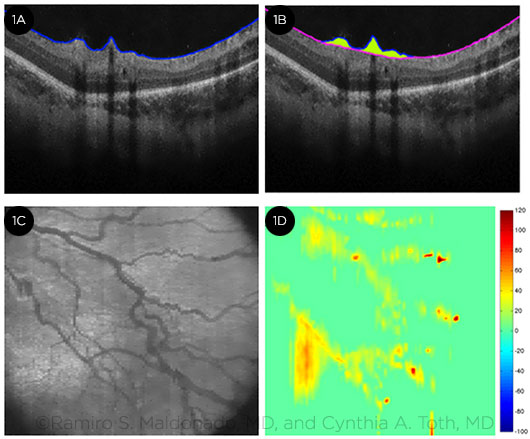
VESSEL ELEVATION. Measurement of vessel elevation over retinal surface (indirect marker of dilation and tortuosity) in a premature infant with ROP. (1A) Automatic segmentation of internal limiting membrane. (1B) Automatic measurement of area above retinal surface. (1C) Summed-voxel projection image comparable to a gray-tone fundus photo, showing tortuous vessels. (1D) Color-thickness map of retinal vessel elevation (extrapolated from a volumetric scan).
|
Expanding Applications
Diagnostic capabilities. Handheld OCT is “an excellent diagnostic tool for [younger] children,” said Mays A. El-Dairi, MD, at Duke University. “We cannot get a proper visual field before age 8, and we cannot use a tabletop OCT before age 3. Furthermore, children often are not able to describe their decrease in vision. Handheld OCT allows us to both diagnose children and follow the changes in their eye disease noninvasively over time.”
And Mary Elizabeth Hartnett, MD, at the University of Utah, noted that she has found handheld OCT to be particularly useful for viewing the structure of the macula. She uses it regularly in her university’s busy neonatal ICU, which is located in a catchment area for rural communities in the expansive Intermountain West.
Research targets. Areas currently under investigation for the handheld device include retinopathy of prematurity (ROP),2 macular edema of prematurity,3 retinal dystrophies and degenerations, and diseases of the optic nerve. Handheld OCT also may be able to validate imaging markers of vascular dilation and tortuosity in retinal vascular diseases,4 commented Ramiro S. Maldonado, MD, at Duke University (Figs. 1A-1D).
Dr. El-Dairi and her colleagues have used handheld OCT to measure and describe the average retinal nerve fiber layer thickness in both full-term and premature neonates,5,6 and Duke researchers also have found SD-OCT imaging markers in the retinas of premature infants that could potentially predict poorer neurodevelopment.7
With regard to ROP, J. Timothy Stout, MD, PhD, MBA, at Baylor College of Medicine, has found handheld OCT to be a valuable tool in examining and following infants with the disease. Now that bevacizumab (Avastin) is being used more often for cases of ROP, “occasionally, we will see progressive vitreoretinal traction as a consequence” of treatment with the drug, Dr. Stout said. “OCT helps us define the areas of traction.”
Dr. Stout added that handheld OCT is also useful for following children who have inflammatory disease or have suffered ocular trauma.
 |
|
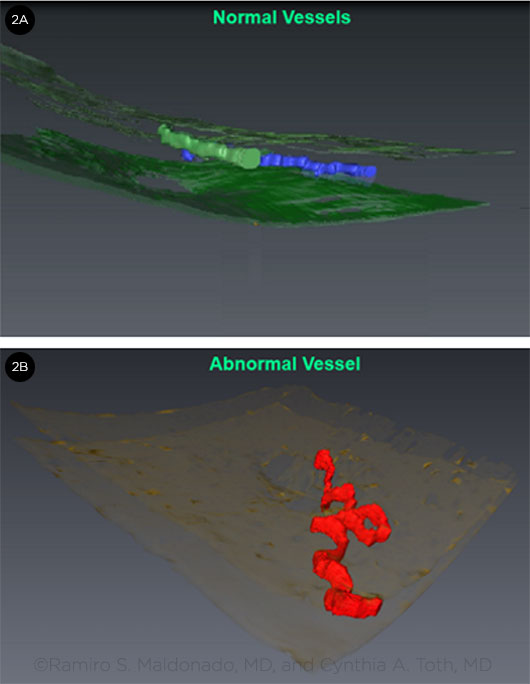
3-DIMENSIONAL IMAGING. Volume-rendering techniques from SD-OCT scans obtained from a premature infant with ROP (2A) and with ROP and plus disease (2B) were used to create this 3-D reconstruction of retinal vessels.
|
Clinical Challenges
The experts noted several challenges with using OCT in children.
Learning curve. Dr. Hartnett and her ophthalmic photographer attended a course at Duke University on how to use handheld OCT on premature babies. “The learning curve is a little longer than other devices,” she said. “With the handheld device, it is important to be sure it is stabilized and that you are using the right reference settings. I work a lot with ophthalmic photographers, who can troubleshoot artifacts.”
“There is definitely a learning curve—and, initially, it is difficult to get the image in focus,” Dr. Stout agreed. “However, [using the device] eventually becomes second nature.”
Interpretation. At present, most OCT systems used in the clinical setting are the familiar tabletop units, not handheld units. In either event, clinicians need to know how to use the technology correctly and to take care in interpreting the results, said Dr. El-Dairi (see “Customized Settings Prove Key” below).
Exam Tips
Tabletop OCT. For a successful exam, Dr. Edmond and her ophthalmic photographer recommended the following techniques.
- Use eye-tracking technology. This allows a child to look away from the fixation target briefly—and often—and still complete the scan with good results.
- Provide distractions. These include singing with the child or having the child use the eye that is not being scanned to look at the photographer.
- Take a team approach. An additional technician may be needed to help distract the child long enough for the photographer to obtain an image.
- Provide reassurance. More often than not, once the child realizes that the photographer is telling the truth when he or she says “I’m not going to touch your eye at all” or “all you have to do is look at a pretty blue light,” the child can relax and cooperate.
Handheld OCT. Young patients who are unable to undergo a tabletop OCT are candidates for the handheld device. This category includes not only preemies but also infants, toddlers, and any child who is uncooperative or who has developmental delays.
- Use a helper. A “helper or two” is definitely required if you are using the handheld OCT, Dr. Edmond said.
- Skip the speculum and drops. When handheld OCT scans are captured on premature babies or infants who are awake, “we do not need to use an eyelid speculum or dilation eyedrops,” Dr. Maldonado said. “Premature eyes are delicate, so we gently open the eyelids and get the scan in 6 seconds. With babies and toddlers who are not sedated or under anesthesia, we use the same approach but may need to take a couple of scans to obtain the specific image we are seeking.”
- Be prepared. “The key point is to be fast and efficient,” Dr. Maldonado added. “Before we start the imaging session, we need to have the system’s reference arm, the probe lens, and the scanning parameters set according to the patient’s age so that we don’t lose precious time.”
Future Applications
Dr. Maldonado cautioned that OCT does not replace ophthalmoscopy or fundus photography, “but it is certainly a complement, and we are still in the early stages of discovering more about the pediatric eye with handheld OCT.”
Dr. Hartnett, who studies the mechanisms of normal and aberrant angiogenesis related to ROP, said that handheld SD-OCT may prove useful in her experimental gene therapy studies. “For example, we can see postinjection if interventions in experimental models affect the structure or function of the retina over time,” she said. “In the meantime, in a child who has reduced vision and you can’t determine why, OCT can be helpful in pointing you in the right direction in terms of diagnosis,” she added. “The handheld OCT is very useful for young children and infants who cannot cooperate for a clinical examination, but don’t assume that a young child can’t sit still for an OCT in clinic. It is often worth giving it a try.”
___________________________
1 Scott AW et al. Am J Ophthalmol. 2009;147(2):364-373.
2 Maldonado RS, Toth CA. Clin Perinatol. 2013;40(2):271-296.
3 Maldonado RS et al. Arch Ophthalmol. 2012;130(5):569-578.
4 Maldonado RS et al. Ophthalmology. 2014;121(6):1289-1296.
5 Rothman AL et al. Am J Ophthalmol. 2015;159(4):803-811.
6 Rothman AL et al. Am J Ophthalmol. 2015;160(6):1296-1308.e2.
7 Rothman AL et al. Ophthalmology. 2015;122(3);610-619.
___________________________
Dr. Edmond is associate professor of ophthalmology and pediatrics at Baylor College of Medicine and a pediatric care specialist at the Texas Children’s Hospital in Houston. Relevant financial disclosures: Alcon, L.
Dr. El-Dairi is assistant professor of ophthalmology at Duke University School of Medicine in Durham, N.C. Relevant financial disclosures: Knights Templar Eye Foundation: S; Pranabio: C.
Dr. Hartnett is professor of ophthalmology and visual sciences and adjunct professor of pediatrics and neurobiology and anatomy at the University of Utah in Salt Lake City. Relevant financial disclosures: March of Dimes: S; National Eye Institute: S.
Dr. Maldonado is an ophthalmology resident at Duke University Eye Center in Durham, N.C. Relevant financial disclosures: None.
Dr. Stout is the Sid W. Richardson Professor of Ophthalmology and the Margarett Root Brown Chair of Ophthalmology at Baylor College of Medicine and director of the Cullen Eye Institute in Houston. Relevant financial disclosures: None.
See the disclosure key at www.aao.org/eyenet/disclosures.