By Jill Wells, MD, William Pearce, MD, John Payne, MD, and Steven Yeh, MD
Edited by Steven J. Gedde, MD
Download PDF
Pamela Peacock,* a 33-year-old bipolar woman, was 14 weeks pregnant when she started suffering a mild headache. At 30 weeks of pregnancy, she noticed that vision in her left eye became blurry. After 2 days of blurred vision, she visited her local optometrist, who noted papilledema and sent her to the emergency room.
She Visits the ER
While in the ER, she complained of seeing blurry spots near the center of her vision in the left eye. An ophthalmology resident examined Ms. Peacock and found the following:
- Visual acuity was 20/20 in each eye.
- There was no relative afferent pupillary defect.
- Color plates were normal.
- Confrontation visual fields were full, although she noted 3 dark spots moving around while looking centrally out of the left eye.
- Motility was normal.
- Anterior segment exam was normal.
- Intraocular pressure was 15 mm Hg in both eyes.
- Optic nerves were pink with indistinct margins; there were no disc hemorrhages and no blurring of the vessels.
- Macula, retinal vessels, and periphery appeared normal in both eyes.
Because her history included chronic headache and questionable papilledema, neurology ordered magnetic resonance imaging and magnetic resonance venography. These showed focal narrowing of the lateral right transverse sinus, and a nonocclusive thrombus could not be excluded. Because of the supposed papilledema (diagnosed by the referring optometrist), the neurology team decided to obtain a lumbar puncture. The opening pressure was 12 mm Hg.
Ms. Peacock was admitted to the hospital overnight.
We Get a Look
The following morning, we saw Ms. Peacock and confirmed the ophthalmology resident’s findings.
Given her normal opening pressure, only a small focal narrowing of the transverse sinus, and—despite the optometrist’s observation—no obvious sign of papilledema, we believed that her symptoms were not related to increased intracranial hypertension. She underwent Humphrey visual field testing, as an inpatient, which showed a full field in the right eye and a small paracentral scotoma in the left.
Differential Diagnosis
At this point, the diagnosis was not clear, given her vision of 20/20 and the normal fundus appearance.
The differential diagnosis included an optic neuropathy versus retinopathy. After considering her normal visual field in the right eye, paracentral scotoma in the left eye, and lack of a relative afferent pupillary defect, we believed a maculopathy was more likely. With that in mind, we now included central serous retinopathy, retinal migraine, acute macular neuroretinopathy, and unilateral acute idiopathic maculopathy in our differential diagnosis.
Follow-up
Ms. Peacock was discharged from the hospital and followed as an outpatient for further imaging.
She returned 2 weeks later, and although she reported that her headache had resolved, the blurry spots in her left eye were worse. Her vision was 20/20 in both eyes. On dilated fundus exam, she had very subtle, deep hyperpigmented spots near the fovea in her left eye. OCT showed normal architecture in the right eye and attenuation of the ellipsoid layer in the left.
Our Diagnosis
The infrared reflective image on the OCT was what clinched the diagnosis. There were dark petalloid perifoveal lesions with the tips pointed toward the fovea. A rare diagnosis of acute macular neuroretinopathy was established. We recommended observation with follow-up in 1 month, but she did not return to the clinic.
Discussion
Acute macular neuroretinopathy (AMN) was first described by Drs. Bos and Deutman after a series of 4 women presented with acute decline in vision and were found to have paracentral scotomata corresponding to wedge-shaped lesions of the macula.1 Similar to other inflammatory maculopathies, some patients suffer from an antecedent febrile illness before the ocular signs and symptoms develop.
Other case series have implicated medications and illicit drugs as the offending stimulus. A recent review of the literature reported that 90% of patients were female, with an average age at diagnosis of 30 years. Regardless of etiology, the final common disease process includes monocular paracentral scotomata that correspond to discrete petalloid or wedge-shaped lesions near the fovea.2
The diagnosis can be difficult to make, as in our case, because the fundus exam is typically normal at the onset of symptoms. The 2 diagnostic imaging modalities useful in identifying this disease entity are OCT and infrared fundus photography, though the latter isn’t available in many clinics. OCT machines use infrared light to illuminate the macula for the photographer, and this image highlights hyporeflective petalloid lesions better than slit-lamp biomicroscopy or color fundus photography. The OCT may show focal signal reduction of the ellipsoid junction.
Currently, there is no body of evidence to suggest that any therapy—topical or systemic—has a role in reducing disease-related morbidity or accelerating convalescence. Aziz et al. reported that of 32 cases with follow-up, 9 demonstrated complete resolution of symptoms and 19 demonstrated some degree of subjective improvement.3
With further understanding of the disease process through additional reports of cases in the literature, the evidence will continue to expand and allow clinicians to further define this disease spectrum and explore methods for potential prevention and treatment.
___________________________
*Patient name is fictitious.
___________________________
1 Bos PM, Deutman AF. Am J Ophthalmol. 1975;80(4):573-584.
2 Turbeville SD et al. Surv Ophthalmol. 2003;48(1):1-11.
3 Aziz HA et al. Ophthalmic Surg Lasers Imaging Retina. 2015;46(1):114-124.
___________________________
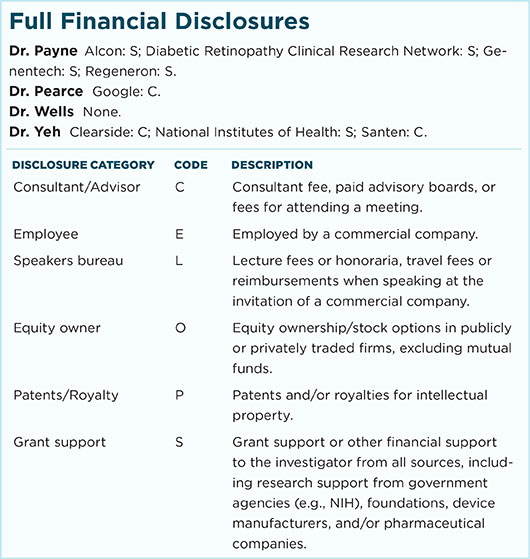
Dr. Wells is a comprehensive ophthalmologist/ ocular oncologist, Dr. Pearce is an ophthalmology resident, and Dr. Yeh is a retina/uveitis specialist; all are at the Emory University Eye Center. Dr. Payne is a retina specialist at the Palmetto Retina Center in Columbia, S.C. Relevant financial disclosures: Drs. Wells and Pearce: None. Dr. Payne: Alcon: S; Diabetic Retinopathy Clinical Research Network: S; Genentech: S; Regeneron: S. Dr. Yeh: Clearside: S; National Institutes of Health: S. Funding was provided by an unrestricted departmental grant from Research to Prevent Blindness.
For full disclosures and the disclosure key, see below.