By Mike Mott, Contributing Writer, interviewing Gregg T. Kokame, MD, MMM, William E. Smiddy, MD, and Jayanth S. Sridhar, MD
Download PDF
In recent years, many cataract surgeons have moved toward polytetrafluoroethylene (Gore-Tex) as their go-to suture for the scleral fixation of posterior chamber IOLs (PCIOLs) in eyes with inadequate capsular support. Concern with the long-term durability of polypropylene (Prolene) has helped to quicken this shift, especially for managing postoperative IOL dislocation. But is it wise for ophthalmologists to ignore Prolene altogether as a suture option? Recent research reopens the discussion.
Prolene’s Strengths
Cataract surgeons have been using Prolene sutures successfully for IOL fixation since 1988; however, an influential 2006 study from the Moorfields Eye Hospital found the 10-0 gauge Prolene to be less durable than expected following transscleral suture fixation of PCIOLs.1 It showed a breakage rate of close to 28% and a mean interval between fixation and breakage of 50 ± 28 months. These findings, combined with similar subsequent reports, led to recommendations for Gore-Tex as the preferred alternative and using only the thicker-gauge 9-0 Prolene variant if the material was to be used at all.2 Many ophthalmologists have taken these recommendations to heart.
Experience proves otherwise. But for other surgeons, the results of these studies simply have not matched up with their own experience. “This literature highlights Prolene’s supposedly high rate of breakage and dissolution,” said William E. Smiddy, MD, at the Bascom Palmer Eye Institute in Miami. “But simply put, that’s just not my experience, nor [that of] my colleagues, who have been using the material for quite a number of years.”
It might benefit ophthalmologists to consider whether the reported high breakage rates are due to their surgical technique rather than the suture material itself, said Dr. Smiddy. “I’m not denying that Prolene might somehow or another fail, but in my more than 30 years using the material, I’ve not witnessed anything close to those reported failure rates. Typically, if the suture breaks, it has to do with knot instability—for example, the surgeon might overtie the suture on the table.”
New data. Research by Gregg T. Kokame, MD, MMM, at the University of Hawai’i, also refutes earlier conclusions regarding Prolene’s weaknesses.3 In a 2018 single-surgeon, retrospective study of 111 patients, his team assessed whether 10-0 Prolene can provide long-term success for dislocated PCIOLs or secondary scleral-fixated PCIOLs. The results were very much at odds with the 2006 Moorfields report. Not only was the breakage rate less than 0.5% (one case in 214 fixation sutures), the researchers also documented suture stability for up to 24 years.
Dr. Kokame hopes these newer findings can help to dispel the idea that “Gore-Tex is gospel.” He noted, “Gore-Tex is a reasonable suture, but some of the information regarding the use of Prolene needs to be updated. For physicians, in general, it’s common to fixate on one particular study, such as the Moorfields study, that’s become repeatedly quoted, rather than embrace the steady stream of new research showing more recent data. And we’ve witnessed this in ophthalmology, where surgeons are abandoning the use of Prolene. But our study demonstrates that it can be a very stable suture that lasts a long time.”
 |
|
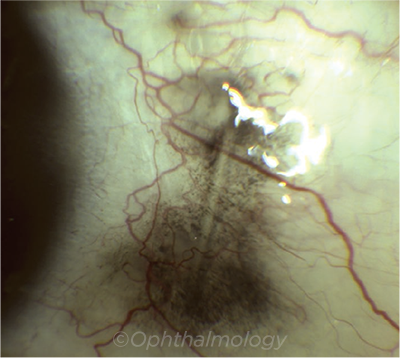
REACTION. Hyperpigmentation adjacent to subconjunctival Gore-Tex.
|
A Look at Gore-Tex
“The debate about Prolene versus Gore-Tex really highlights the fact that there are many different ways to achieve a positive surgical outcome,” said Jayanth S. Sridhar, MD, at the Bascom Palmer Eye Institute. “I use both materials but not with the same frequency. In the rare case where I am rescuing an IOL and suturing it to the iris, I will opt for Prolene. But for the most part, I use Gore-Tex.” And there’s likely a generational component as to who uses what suture material and why, he added. “I trained at a program in which most sutured IOLs involved Gore-Tex, and that’s carried over into my practice. But in the right hands, both sutures are very useful as long you are aware of their advantages and disadvantages.”
Bury knots carefully. Surgeons will note differences in how the sutures behave intraoperatively. Prolene is a finer, more typical suture material whereas Gore-Tex is thicker, bulkier, and more pliable, and it has “memory.” The characteristics of the latter do allow for easy manipulation and more secure knot-tying, said Dr. Sridhar, but they also can make it more difficult to bury the suture knot in the sclera, a critical step. “Gore-Tex potentially has a higher risk of exposure because the bulky knot can erode through the conjunctiva over time. So it’s imperative to bury your tied-off knots adequately to prevent exposure to the conjunctiva and possible infection.”
Nonreactive? For the most part, however, it’s been theorized that the soft, microporous nature of Gore-Tex should lead to nonreactivity and minimal inflammatory response. In fact, recent studies have shown favorable outcomes without severe complications, and, indeed, Gore-Tex has been used successfully in cardiovascular surgery for a number of years.4,5
But, as Dr. Kokame notes, there are some new reports highlighting possible concerns with its use: for example, suture-related infection requiring removal of the IOL,6 eyelet fracture secondary to tension from a Gore-Tex suture,7 and hyperpigmentary reaction adjacent to the subconjunctival suture.8 “I don’t believe Gore-Tex is as nonreactive as initially billed,” said Dr. Kokame. “With any new advancement in ophthalmic surgery, the more follow-up we have, the more we’ll be able to identify reactions over time. But Gore-Tex is not labeled for ophthalmic use and doesn’t have the large prospective studies confirming any long-term complication profiles.”
Track record. Dr. Sridhar agrees that Gore-Tex’s shorter duration of use in ophthalmic surgery makes it more difficult to assess the material’s long-term efficacy. “At this point in time, we’re just assuming that scleral-fixated IOLs using Gore-Tex will perform well 15, 20, 25 years down the road,” he said. “But we just don’t have the track record to say that with 100% certainty. No one can accurately say, ‘Gore-Tex is definitely going to last longer than Prolene,’ because we don’t have that real-world data. Yes, I’m confident in my use of Gore-Tex—I’ve witnessed, first-hand, plenty of dislocated Prolene-sutured lenses that I refixated with Gore-Tex. But our long-term understanding of the material is based on theory and from other fields. We don’t have the data from ophthalmology. We have data from the vascular surgery literature.”
Managing the dislocated lens. It’s also important to realize that your suture choice can ultimately affect your surgical choice when addressing IOL dislocation, said Dr. Smiddy. “I certainly would never condemn the use of Gore-Tex. It’s a fantastic option. But ophthalmologists should be aware that if you’re going to use that material, you’re generally going to manage dislocated IOLs a bit differently.”
Using Prolene, for example, can allow the cataract surgeon to reposition the existing lens implant. And research from Dr. Smiddy and colleagues has demonstrated both good outcomes and low complication rates with this technique.9 Gore-Tex, on the other hand, generally constrains the surgeon to perform an IOL exchange—a generally easier but potentially more complicated and invasive procedure.
“In the zeal for a stronger suturing device, we might be inadvertently promoting IOL exchange and abandoning IOL repositioning,” said Dr. Smiddy. “And in my opinion, if you don’t have to come through the anterior segment again to remove and reinsert an IOL, you’ve made for a smaller operation with less fallout in terms of corneal endothelial loss or complications with existing corneal transplants or glaucoma, for example.”
Keep Your Options Open
The newly published Academy Ophthalmic Technology Assessment (OTA) on implanting IOLs in the absence of zonular support has concluded that surgeons need to be adroit in several different types of IOL fixation techniques given each unique patient case (aao.org/ota).10 And although the OTA doesn’t include an assessment of Prolene’s strengths, the Academy’s recommendation does include iris-and scleral-sutured fixation of PCIOLs using the 10-0 variant.
Dr. Smiddy agrees with the OTA’s conclusion. “The ophthalmic community shouldn’t coin the Prolene versus Gore-Tex debate in terms of good and bad. The debate will continue because there’s no clear and current evidence that one is significantly better than the other. We should instead embrace the fact that we have different options for managing different patients to produce the best surgical results.”
___________________________
1 Vote BJ et al. Am J Ophthalmol. 2006;141(2):308-312.
2 McAllister AS, Hirst LW. J Cataract Refract Surg. 2011;37(7):1263-1269.
3 Kokame GT et al. Am J Ophthalmol. 2018;189(5):10-116.
4 Khan MA et al. Retina. 2018;38(7):1377-1384.
5 Khan MA et al. Retina. 2019;39(5):860-866.
6 Patel NA et al. Clin Ophthalmol. 2018;12:1245-2148.
7 Gupta RR et al. J Vitreoretin Dis. 2019;3(5):395-398.
8 Chen X et al. Ophthalmology. 2018;125(6):841.
9 Kim SS et al. Ophthalmology. 2008;115(10):1699-1704.
10 Shen JF et al. Ophthalmology. Published online June 5, 2020.
___________________________
Dr. Kokame is clinical professor and chief of ophthalmology at the University of Hawai’i John A. Burns School of Medicine in Honolulu. Relevant financial disclosures: None.
Dr. Smiddy is professor of ophthalmology and the M. Brenn Green Chair in Ophthalmology at the Bascom Palmer Eye Institute in Miami. Relevant financial disclosures: None.
Dr. Sridhar is associate professor of clinical ophthalmology at the Bascom Palmer Eye Institute. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Kokame Bayer Healthcare: C; Genentech: S; Iveric: S; Novartis: S; Regeneron: C,S; Salutaris: S; Zeiss: C.
Dr. Smiddy None
Dr. Sridhar Alcon: C; Alimera: C; Allergan: C.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|