By Lori Baker-Schena, MBA, EdD, interviewing Rubens Belfort Jr., MD, PhD, Debra A. Goldstein, MD, Cynthia Moore, MD, PhD, and Steven Yeh, MD
Download PDF
In December 2015, Rubens Belfort Jr., MD, PhD, of the Federal University of São Paulo, Brazil, and colleagues traveled northeast to Salvador, Brazil, to evaluate 29 infants with microcephaly with a presumed diagnosis of congenital Zika virus. Less than 6 weeks later, their findings were published in the Feb. 9, 2016, online edition of JAMA Ophthalmology1—reflecting both the urgent need to study the growing epidemic and the vital role of the ophthalmic community in addressing its challenges.
Disturbing Signs
“Zika virus appeared in Brazil in April 2015 seemingly out of nowhere,” Dr. Belfort said. “Given the vision issues associated with infectious diseases such as cytomegalovirus, rubella, syphilis, and toxoplasmosis, we anticipated that we would find ocular abnormalities as well in infants with microcephaly associated with presumed intrauterine Zika infection.”
First reports. Dr. Belfort and his team sprang into action, publishing the first report of possible congenital ocular lesions in 3 infants from Recife, Pernambuco, Brazil, online in the Lancet on Jan. 7, 2016,2 closely followed by a report in the Arquivos Brasileiros de Oftalmologia3 describing 10 infants examined in Recife who were born with presumed Zika virus–related microcephaly presenting with macular and optic nerve abnormalities.
“In both Brazilian cities, Salvador and Recife, we saw the same distinctive profile for the ocular abnormalities in these infants,” Dr. Belfort said. In the JAMA Ophthalmology article, he and his coauthors described the abnormalities as “ocular lesions consisting of focal pigment mottling and chorioretinal atrophy with a predilection for the posterior pole, especially the macular area, as well as optic disc abnormalities.”
Dr. Belfort said that while additional studies and improved serologic tests are necessary to confirm a cause-and-effect relationship between the Zika virus and these ocular abnormalities, his team’s findings can help “guide clinical management and practice” in the meantime.
 |
|
MICROCEPHALY AND THE RETINA. (1) Photograph of microcephalic infant who has retinal and optic nerve lesions. (2) Funduscopy of the left eye (different patient) presenting pale optic nerve head, large cup-disc ratio, and 2 confluent nasal lesions, suggestive of severe chorioretinal atrophy, surrounded by hyperpigmented mottling.
|
Crisis Unfolding at Startling Speed
In May 2015, the Pan American Health Organization issued an alert regarding the first confirmed Zika virus infection in Brazil. By Dec. 10, 2015, the Zika virus had spread to more than 18 Brazilian states and had rapidly became an epidemic, especially in northeastern Brazil.1 It has since expanded to several other tropical countries, with the U.S. Centers for Disease Control and Prevention (CDC) regularly adding more to the list (www.cdc.gov/zika/geo).
Throughout the last few months, the worldwide urgency to address the Zika virus has been vividly apparent—from the frequently updated guidelines issued by the CDC (see “Guidelines for Ophthalmologists”) to the daily reports in the lay press to the growing number of peer-reviewed articles across medical specialties.
Transmission of the virus. Zika virus is a flavivirus transmitted primarily through the bite of an infected Aedes aegypti mosquito—the same mosquito that transmits dengue, chikungunya, and yellow fever.4 The most common symptoms of Zika are fever, rash, joint pain, and conjunctivitis.
In addition, there may be other modes of transmission apart from mosquito bites. “Recent information coming from different countries and the WHO [World Health Organization] has stressed the possibility of this infection also being transmitted sexually,” Dr. Belfort noted. “The risk of pregnant women acquiring Zika this way and of the fetus developing microcephaly has prompted authorities to suggest the use of condoms in places with higher risk.”
Distinctive Ocular Findings
In the Salvador study, researchers observed ocular abnormalities in 10 of the 29 infants born with microcephaly associated with presumed intrauterine Zika.1 The most common ocular lesions were focal pigment mottling and chorioretinal atrophy. Dr. Belfort noted that 2 of the ocular abnormalities seen with the Zika virus were distinctive: circumscribed areas of chorioretinal atrophy, which in some areas had no choroidal vessels visible at all; and circumscribed areas of pigmentary clumping. Given that these retinal lesions differed from those previously reported in other congenital infections, the authors hypothesized that a cause-and-effect relationship between the Zika virus infection and ocular abnormalities was possible. However, more studies and advances in diagnostic testing are necessary.
Is Zika the cause? Indeed, while the Zika virus link to retinal lesions in microcephalic infants is compelling, it is not currently definitive. JAMA Ophthalmology invited Lee M. Jampol, MD, and Debra A. Goldstein, MD, of Northwestern University to author an editorial detailing the challenges of establishing causation.5 The commentary noted microcephaly may have several causes, and definitive serological testing for Zika virus was not available in Brazil at the time of the original outbreak.
“I think the epidemiologic evidence is very convincing that the outbreak of microcephaly in Brazil is related to the outbreak of the Zika virus infection,” Dr. Goldstein said. “The difficulty with ascertainment early on was that the Zika infection itself may be very mild, so it was not initially reported.”
“In light of the increased knowledge of risks associated with Zika, pregnant women are now reporting symptoms of infection,” she added. “This makes testing of mothers possible during the active phase of infection. However, as good serological testing is still not available given the cross-reactivity with other infections, diagnosis relies primarily on PCR [polymerase chain reaction], which remains positive for only a short period of time.”
(Story continues below.)
Guidelines for Ophthalmologists
As of Feb. 23, 2016, vector-borne transmission of Zika virus had not been identified in any of the 50 states, but it has occurred in U.S. territories, according to CDC. While the U.S. mainland does have Aedes species mosquitoes that can become infected with and spread Zika virus, all cases in the United States are associated with travel. Most states with Zika have fewer than 6 cases, and most of those have only 1 case. Florida, New York, and Texas have 28, 17, and 13 cases, respectively.1
As an arboviral disease, Zika is nationally notifiable, and health care providers are asked to report suspected cases to their state or local health departments to facilitate diagnosis and mitigate the risk of local transmission. The Jan. 29 CDC Mortality and Morbidity Weekly Report2 also recommended Zika virus testing “for 1) infants with microcephaly or intracranial calcifications born to women who traveled to or resided in an area with Zika virus transmission while pregnant; or 2) infants born to mothers with positive or inconclusive test results for Zika virus infection.” (The CDC’s guidelines for collection and submission of body fluids for Zika virus testing can be found at www.cdc.gov/zika/hc-providers/body-fluids-collection-submission.html.)
According to the Academy’s Clinical Statement on Zika, the CDC also recommends that as part of an examination of infants with possible congenital Zika virus infection, an eye exam be performed, including a retina evaluation, either in the hospital or within 1 month after birth.
The CDC is frequently updating its guidelines, a task made more formidable by a shifting information landscape. “We traditionally depend on data to develop evidence-based guidelines,” noted Cynthia Moore, MD, PhD, director of the Division of Congenital and Developmental Disorders in the CDC National Center on Birth Defects and Developmental Disabilities, and subject matter expert for the 2016 CDC Zika Virus Response Team.
“However, with emerging diseases such as Zika virus disease, we have to develop our interim guidelines through a combination of evidence-based information and guidance from experts in the clinical community, including subspecialists within the American Academy of Pediatrics,” she said.
Dr. Moore added that the CDC is working to develop and expand Zika laboratory testing capacity and to conduct studies focused on the link between Zika and microcephaly and GBS.
For more information, visit the CDC recommendations for physicians at www.cdc.gov/zika/hc-providers/index.html and the Academy’s Clinical Statement at www.aao.org/clinical-statement/zika-virus-infection-potential-ophthalmic-manifest.
___________________________
1 www.cdc.gov/zika/geo/index.html.
2 www.cdc.gov/mmwr/volumes/65/wr/mm6503e3.htm.
|
Apparent Guillain-Barré–Zika Virus Link
The apparent link between the Zika virus and an increase in the number of Guillain-Barré syndrome (GBS) cases in 6 counties or territories (Brazil, French Polynesia, Colombia, El Salvador, Suriname, and Venezuela) is also of concern to ophthalmologists. A growing body of evidence is pointing to a causal role for Zika in GBS. Notably, 1 case control study showed that 98% of GBS study patients (n = 42) had anti–Zika virus IgM or IgG, and 100% had neutralizing antibodies against Zika, compared with 56% in the control group (p < .0001).6
Understand effects on the eye. Steven Yeh, MD, of the Emory Eye Center in Atlanta, is no stranger to devastating viruses. He was on the ophthalmology team that detected viable Ebola virus in the aqueous humor of a patient recovering from Ebola virus disease who had presented with acute panuveitis several months following hospital discharge.7
“As the world increasingly becomes more connected, it is vital for ophthalmologists to keep informed of the ocular ramifications of these viral outbreaks—which have the potential to come to our shores,” Dr. Yeh said. “For example, our team in conjunction with NGOs and other partners found that up to 20% of Ebola survivors may develop uveitis, demonstrating a strong link between viral infection and ophthalmic disease that is important to recognize.”
Miller Fisher syndrome. Dr. Yeh said the possible linkage between Zika virus and GBS should be noted by ophthalmologists particularly because one variant of GBS is Miller Fisher syndrome, which is characterized by multiple oculomotor palsies. “The link between Zika and GBS is currently under investigation. The Miller Fisher subtype of GBS has not been identified thus far in association with Zika but should also be a consideration,” Dr. Yeh said.
“With summer and warmer weather coming and the accompanying rise in the mosquito population—especially in the Southern United States—it is vital for ophthalmologists to stay current with the latest discoveries related to the Zika virus,” Dr. Yeh added.
A Continually Evolving Situation
Dr. Belfort noted that one of the frustrations faced by researchers in Brazil is the high cost of examining these infants. “We utilize the same equipment used to study ROP [retinopathy of prematurity], and these cameras cost $80,000 each,” Dr. Belfort said. “In a region like northeast Brazil, we need at least 20 cameras just to begin.”
Dr. Goldstein agreed, “There is already a huge burden on available resources, and screening is not likely to be practical for all babies born in endemic areas, so [it] will, for the time being at least, be restricted to microcephalic babies or to mothers with suspected infection during pregnancy.”
More questions. But what about those infants who appear normal at birth but whose mothers were infected with Zika virus? Dr. Belfort suspects that they may develop subsequent vision problems as they grow, and he is planning to research this possibility.
Dr. Goldstein added, “It is certainly possible that Zika infection can have a spectrum of in utero sequelae and that infection in the third trimester might result in retinal or other findings in the absence of microcephaly or other major developmental issues. Since screening is taking place only on microcephalic babies, these findings will likely not be picked up until later, potentially presenting as decreased vision or strabismus,” she said. “Unfortunately, the true impact of the Zika virus infection on developing fetuses is not yet known, and the spectrum of developmental abnormalities is likely to expand.”
___________________________
1 de Paula Freitas B et al. JAMA Ophthalmol. Published online Feb. 9, 2016.
2 Ventura CV et al. Lancet. 2016;387(10015):228.
3 Ventura CV et al. Arq Bras Oftalmol. 2016;79(1):1-3.
4 www.aao.org/clinical-statement/zika-virus-infection-potential-ophthalmic-manifest. Accessed Feb. 29, 2016.
5 Jampol LM, Goldstein DA. JAMA Ophthalmol. Published online Feb. 9, 2016.
6 Cao-Lormeau VM et al. Lancet. Published online Feb. 29, 2016.
7 Varkey JB et al. N Engl J Med. 2015;372(25):2423-2427.
___________________________
Dr. Belfort is the head professor of ophthalmology at the Federal University of São Paulo, Brazil, and president of the Brazilian Academy of Ophthalmology. Relevant financial disclosures: None.
Dr. Goldstein is a professor of ophthalmology and director, Uveitis Service and Uveitis Fellowship, in the Department of Ophthalmology at the Northwestern University Feinberg School of Medicine, in Chicago. Relevant financial disclosures: None.
Dr. Moore is director of the Division of Congenital and Developmental Disorders in the CDC National Center on Birth Defects and Developmental Disabilities. Relevant financial disclosures: None.
Dr. Yeh is the Louise M. Simpson Professor of Ophthalmology, section of Vitreoretinal Surgery and Diseases, director of the Section of Uveitis and Vasculitis, at the Emory Eye Center, Emory University, Atlanta. Relevant financial disclosures: None.
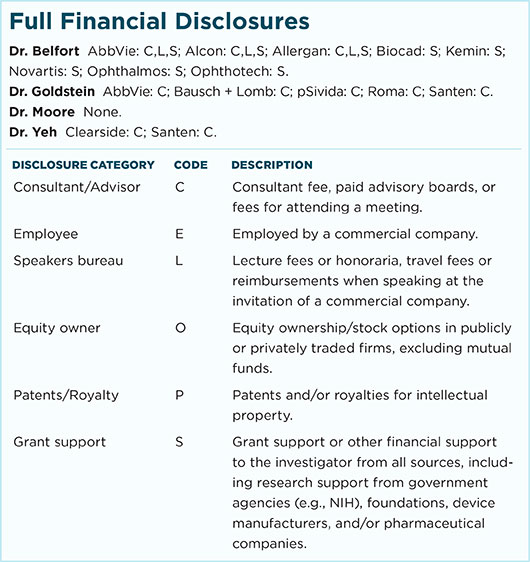
For full disclosures and the disclosure key, see below.