What’s the best way to treat negative dysphotopsia? Prevent it, says Samuel Masket, MD, clinical professor of ophthalmology at the Jules Stein Eye Institute.
Dr. Masket has developed a new IOL, the Morcher 90S IOL, designed to prevent negative dysphotopsia, the dark or grey arc-shaped shadow seen in the temporal field of vision following uncomplicated cataract surgery.
Studies show negative dysphotopsia can be prevented or reversed if the optic edge overlies the anterior capsule. Dr. Masket’s anti-dysphotopsia IOL has a groove on the anterior optic surface that allows the optic to overlap the anterior capsulotomy, instead of the capsule overlying the optic.
Additionally, with the groove in the optic held firmly by the anterior capsulotomy, the IOL is stable and well-centered, he said. The design allows for routine surgery and in-the-bag IOL placement. It can accommodate any haptic or edge design, as well as toric and multifocal designs.
Dr. Masket presented data at ESCRS 2015 that show the new design may prevent this troublesome phenomenon. None of the 39 patients implanted with the lens experienced negative dysphotopsia. Follow-up ranged from 6 to 24 months.
Of the 39 cases, 29 were implanted using a femtosecond laser; 10, were performed manually. The lens failed to capture the capsulotomy in 2 cases, 3 patients had capsule block (fenestrations were later added to the lens to allow fluid egress) and no patients had iris chafe.
While the lens is well-suited for a femtosecond laser-created capsulotomy, he said a manual rhexis also works well.
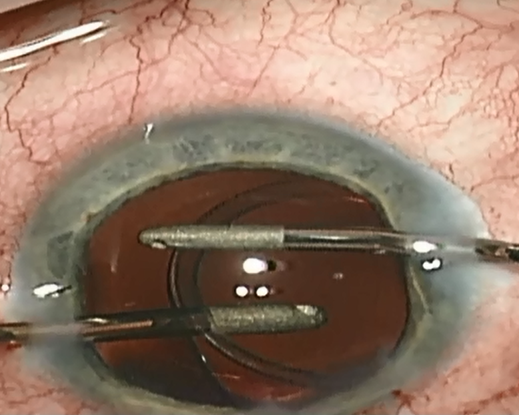
View Burkhard Dick, MD, implant the Morcher 90S during femtosecond laser cataract surgery.
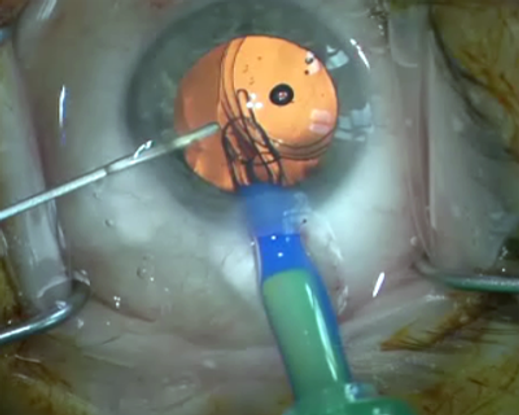
View Oliver Findl, MD, implant the Morcher 90S with manual surgery.
Dr. Masket presented his data at a well-attended symposium dedicated to dysphotopsia. The general consensus was that dysphotopsia is on the rise and is the main cause of dissatisfaction following “routine” cataract surgery.
The immediate postop incidence appears to be about 20%, which is usually best left to resolve on its own. However, published reports show it persists in 1.6% to 3.2% of patients. Given the annual rate of cataract surgery in the United States that translates to 30,000 to 100,000 new patients with negative dysphotopsia each year in the United States alone.
Dr. Masket said there is a lot of misinformation about what causes negative dysphotopsia. Using data from published reports, he debunked several common suppositions: It’s not caused by square-edged acrylic IOLs, ciliary sulcus IOLs or anterior chamber IOLs; the expanded depth of the posterior chamber after cataract surgery is not to blame nor are temporal clear corneal incisions and the IOL position doesn’t matter.
If symptoms don’t resolve by 3 months, surgery is an option. In his experience treating 47 eyes, Dr. Masket said reverse optic capture can be successful, as can IOL exchange, and he has had some success with piggyback IOLs, which he attributes to light diffusion.
Though physicians can’t predict who will develop negative dysphotopsia and there are no good questionnaires to measure its severity, Konrad Pesudovs, Foundation Professor and Chair of Optometry and Vision Science at Flinders University in Australia, had this advice:
“Ask the right questions, but also hear the answer. Beware of surgeon bias. Be careful to listen to what they say. We tend to upregulate operable complaints and downgrade the inoperable.”