58-year-old with gradual onset of blurry vision
What is your diagnosis?

The diagnosis is...
![]()

The image is consistent with a diagnosis of nonproliferative diabetic retinopathy (NPDR):
- NPDR is the early stage of diabetic retinopathy.
- Hyperglycemia damages the retinal vasculature, leading to microaneurysms that may rupture or leak and capillary occlusion causing retinal infarction.
- Diabetic retinopathy is a gradually progressive cause of vision loss that affects 1 in 3 patients with diabetes.
What is the role of the primary care or emergency medicine physician?
![]()
- Refer the patient to ophthalmology nonurgently. For diabetic retinopathy screening, refer to ophthalmology within 5 years of diagnosis of type 1 diabetes mellitus and within 1 year of diagnosis of type 2 diabetes.
- Counsel patients on the importance of glycemic control.
- Provide medical management of diabetes, hypertension, and hyperlipidemia.
What is the role of the ophthalmologist?
![]()
- Examine the fundus with a slit-lamp biomicroscope, looking for signs of diabetic retinopathy: microaneurysms, hard exudates, dot-and-blot hemorrhages, cotton-wool spots, and macular edema.
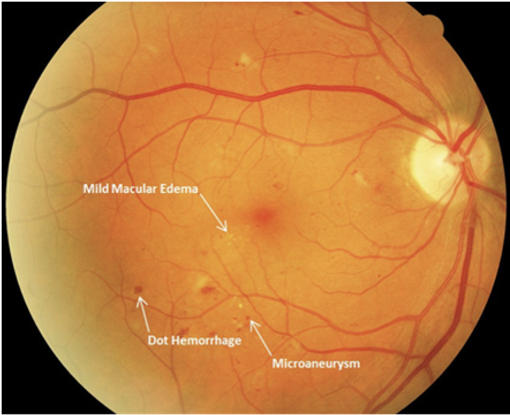
- Assess for retinal neovascularization associated with proliferative diabetic retinopathy.
- Use optical coherence tomography to evaluate macular edema.

What is the treatment?
![]()
Treatment is based on the management of systemic conditions (ie, diabetes, hypertension, hyperlipidemia). Maintaining a hemoglobin A1c level of less than 7% is recommended.
Anti-vascular endothelial growth factor injections can help prevent vision loss in patients with macular edema.
Ophthalmology follow-up should occur every 3-12 months depending on the severity of the diabetic retinopathy.
Learn more: Ophthalmology resources for medical students
![]()