Download PDF
The latest study from DRCR.net delivers important clinical information, but questions remain.
Protocol T, the latest in a string of landmark studies by the Diabetic Retinopathy Clinical Research Network (DRCR.net), adds to a growing body of knowledge that points to anti-VEGF drugs as frontline therapy for center-involved diabetic macular edema (DME).1
At 1 year, all 3 agents in the comparative-effectiveness clinical trial—aflibercept (Eylea), bevacizumab (Avastin), and ranibizumab (Lucentis)—improved vision in eyes with center-involved disease. (The 2-year results are expected in early 2016.) But in a subgroup analysis, aflibercept outperformed the other 2 agents, somewhat complicating the interpretation of results for clinical practice.
“As we see more and more clinical trial data, it provides reassuring evidence of the clear role of anti-VEGF therapy in the management of DME,” said Justis P. Ehlers MD, at the Cleveland Clinic.
Allen C. Ho, MD, of Wills Eye Hospital, concurred. “The results of Protocol T reveal that we can choose between different anti-VEGF agents and do well for our patients, but there are nuances from this head-to-head trial that will impact drug choice.”
Reading the Results
“The most important result is that all 3 drugs were effective at improving vision,” said study coauthor John A. Wells III, MD, of Palmetto Retina Center, in Columbia, S.C. “Overall, Eylea improved vision more, on average, than the other 2 drugs, gaining a mean of 13 letters from baseline versus 11 letters for Lucentis and 10 letters for Avastin.”
Dr. Wells urged caution when interpreting these findings. “If you applied the overall result, you would recommend Eylea for all patients with DME.” But this result, he said, “has limited clinical utility because there was a very strong interaction with baseline visual acuity.” A preplanned subgroup analysis, which compared eyes with better baseline vision of 20/32 to 20/40 against those with baseline vision of 20/50 or worse, found that the overall result was driven by the improvement in the eyes with worse baseline vision. The subgroup analysis, he said, clearly shows that eyes with baseline vision of 20/50 or worse responded best to aflibercept, improving by 19 letters versus 14 letters for ranibizumab and 12 for bevacizumab. Eyes with better baseline vision of 20/32 to 20/40 responded equally to all 3 drugs, improving vision by 8 letters on average. “So the overall result overestimates the benefit of Eylea in eyes with better baseline vision and underestimates the benefit in eyes with worse baseline vision,” said Dr. Wells.
“In previous DRCR DME studies, the median baseline vision has been 20/50,” said Dr. Wells, “so we estimated that would be a good arbitrary point for dividing the eyes into subgroups: better baseline vision of 20/32 to 20/40 and baseline vision of 20/50 or worse. After randomization, each subgroup by chance represented roughly half the eyes enrolled, so our estimate was excellent in creating equal subgroups for comparison.” He said the investigators wanted to look at the response in eyes with worse baseline vision compared to eyes with better baseline vision to test the hypothesis that aflibercept—with possibly the greatest VEGF binding affinity of the 3 drugs—might work better in eyes with worse baseline vision because these eyes possibly have worse DME and higher VEGF levels.
Some considerations. Marco Zarbin, MD, PhD, FACS, at Rutgers–New Jersey Medical School, praised the study’s execution but noted a few concerns.
First, he questions whether the ranibizumab group might have been undertreated. In Protocol T, subjects received a 0.3-mg dose pro re nata (PRN), whereas 0.3 mg of intravitreal ranibizumab has previously been shown to be effective in treating DME when injected on a mandatory monthly basis.2 Also, an earlier study comparing 0.3 mg with 0.5 mg of ranibizumab PRN indicated that 0.3-mg dosing undertreats DME, if given PRN.3
Dr. Zarbin also said, “We need to interpret Protocol T results in the context of other studies.” Specifically, he noted that the ceiling effect, previously observed in earlier randomized clinical studies using ranibizumab and aflibercept for treating DME, was less evident in Protocol T. “In the randomized controlled multicenter studies RIDE, RISE, VIVID, VISTA, RESOLVE, and DRCR.net Protocol I, there was a highly significant negative correlation between mean baseline best-corrected visual acuity and mean best-corrected visual acuity gain. If the Protocol T data are included in the analysis, then the correlation is no longer significant, principally due to the visual results in the aflibercept cohort,” he said.2-5 “Due to these issues, I think we should interpret the results of Protocol T with care, and I look forward to seeing the 2-year visual and anatomic results, which will be available soon,” Dr. Zarbin said.
Other perspectives. Responding to Dr. Zarbin’s concerns, Dr. Ho said, “I would not discount the Protocol T subgroup. It doesn’t put a shadow on T’s findings. It’s something the physician needs to be aware of. It’s a 2-year study, with a 1-year read. We’ll see if that holds through year 2.”
Dr. Ehlers commented that it is important to understand any differences in inclusion/exclusion criteria as well as specific treatment regimens when comparing results across randomized studies. “It is very easy to want to directly compare results, and these comparisons can be highly valuable, but understanding any differences in study cohorts (e.g., chronicity of disease, previous allowed treatment) helps to place those comparisons in better context,” he said.
Dr. Wells responded to several of Dr. Zarbin’s points. He explained that the 0.3-mg dosing for ranibizumab was chosen because it is the FDA-approved dose for DME and that higher adverse events with 0.5 mg were observed in the RISE and RIDE trials. He also noted that some argument may be made for a ceiling effect. “But all 3 drugs could have had a ceiling effect.” As for the outlier argument, he said, “We have a large sample size in each group. The likelihood is low that this result was by chance.”
Protocol T at a Glance
Protocol T randomized 660 adults with center-involved DME to receive IVT therapy. Of these, 224 received 2.0 mg of aflibercept (Eylea), 218 received 1.25 mg of bevacizumab (Avastin), and another 218 received 0.3 mg of ranibizumab (Lucentis). None had received anti-VEGF treatment within the previous 12 months.
At 12 months, visual gains were evaluated on a 0 to 100 letter score, with 85 letters approximating 20/20.
After the baseline treatment, reinjection was performed every 4 weeks, unless deferral criteria were met: VA of 20/20 or better; OCT central subfield thickness less than the normal threshold; and no improvement in, or worsening of, vision or OCT in response to the previous 2 injections. The maximum number of injections was 13.
Improvement was considered to be an increase of 5 or more in the VA letter score (1 Snellen line) and a decrease in central subfield thickness of 10% or more compared with the previous injection. Worsening was defined as a decrease of 5 or more in the VA letter score or an increase in the central subfield thickness of 10% or more from the previous injection.
On average, aflibercept yielded greater visual improvement than the other drugs, though this effect was dependent on baseline VA. The bevacizumab effect was less robust than the other 2 agents, but irrespective of initial VA, few eyes treated with any of these agents had substantial loss of VA.
Some key findings:
- Aflibercept improved vision more, on average, than the other 2 drugs, with +13 letters, compared with +11 for ranibizumab and +10 for bevacizumab.
- In the better vision subgroup—eyes with an initial VA of 20/32 to 20/40 or better (51% of the cohort)—the mean gain at 1 year was 8.0 letters with aflibercept, compared with 7.5 with bevacizumab and 8.3 with ranibizumab.
- In the subgroup with an initial VA of 20/50 or worse, mean improvement at 1 year was 18.9 letters with aflibercept, 11.8 with bevacizumab, and 14.2 with ranibizumab.
- All 3 groups showed improvement in mean VA by 4 weeks. In eyes with worse initial VA, the greater efficacy of aflibercept became apparent as early as 4 weeks.
- The maximum possible number of injections was 13. The median number in the aflibercept group was 9, and it was 10 each in the bevacizumab and ranibizumab groups.
- No difference in systemic or ocular adverse events was observed in any of the groups.
|
Protocol T in the Clinic
Despite the caveats, Protocol T offers a road map for clinical practice. “We now have a more-refined strategy for achieving better outcomes in treating patients with DME,” said study investigator Andreas K. Lauer, MD, at Oregon Health & Science University in Portland. He and the other retina experts spoke about what the findings mean for their clinical practice.
Anti-VEGF as first-line treatment. “My approach to patients is going to change as a result of this study,” said Dr. Wells. In eyes with better vision, he will use bevacizumab or ranibizumab. In patients with 20/50 vision or worse, he noted that he would be likely to treat with aflibercept.
For his patients who are already under control, Dr. Lauer will stay the course. But for new patients with mild vision loss, center-involved DME, and no history of anti-VEGF injections for 12 months, he said that he is comfortable choosing from among the 3 agents.
Dr. Ho would favor starting his center-involved DME patients with ranibizumab or aflibercept. “We know they performed better than Avastin,” he said. “And I may switch between them as a first change in therapy, if response is inadequate.” When insurance issues preclude on-label choices, he uses bevacizumab as a secondary choice. For example, he said, when there are high deductible or high copay scenarios that are not relieved by charity foundations, he will use bevacizumab. More ominously, he added, payers may mandate a specific drug without regard to the individual patient. “It is very important that we fight for drug choice for our patients; our patients count on us to do what is best for them,” he said.
Dr. Zarbin noted that for patients with a recent stroke or heart attack, he would be inclined to use ranibizumab because of its shorter systemic half-life (vs. aflibercept or bevacizumab) after intravitreal injection, as there is a documented reduction in systemic VEGF levels after intravitreal injection of anti-VEGF agents.
Aflibercept for 20/50 or worse. Dr. Wells said that he would be likely to treat with aflibercept in patients with VA of 20/50 or worse because, in that group, eyes treated with aflibercept were 34% more likely to gain 3 lines of vision than eyes treated with ranibizumab, and 63% more likely than with bevacizumab. “I know now that if I use Eylea in a patient with 20/50 or worse vision, I’ll give them a 67% chance of improving 3 lines of vision, compared with a 50% chance with Lucentis, and a 41% chance with Avastin.”
He added, however, that he would use bevacizumab in these eyes if cost is an issue. “The choice of drug is dependent on other factors, such as cost, insurance coverage, and availability of the drugs; and it should be a doctor-patient decision.”
Dr. Zarbin, too, said that he would certainly consider aflibercept, “if the patient is treatment naive and fits the protocol enrollment criteria—particularly if I’m following a PRN posology, and their vision is 20/50 or worse.”
Likewise, Dr. Lauer said that for a patient newly diagnosed with center-involved DME whose visual acuity is 20/50 or worse, he would be inclined to start treatment with aflibercept. “However, if a patient exhibits intolerance or suboptimal response to treatment, or where cost, insurance coverage, or personal preference is a concern, I would consider alternatives to aflibercept—ranibizumab, bevacizumab, or a corticosteroid implant such as dexamethasone [Ozurdex] or fluocinolone [Iluvien],” he said.
Results may vary. Dr. Ho urged ophthalmologists to keep an open mind when considering treatment options. “We’re very lucky to have 3 effective anti-VEGF agents. But remember that variations in individual patient response may lead you to a drug choice that may counter Protocol T results. You’ll do your patients a disservice if you think that drug X works best for all patients.” And if response to anti-VEGF agents is inadequate, corticosteroids are an option, he said.
Caveat for special circumstances. “Regardless of which of the 3 [anti-VEGF] medications are used, we need to exercise caution when considering treatment of DME in patients who are pregnant, who are of child-bearing potential, or who are breast-feeding,” said Dr. Lauer. “We do not know what effect intravitreal anti-VEGF has on developing humans during pregnancy or after birth.”
What Protocol T Means for Laser
“Laser [therapy] was altered years ago by Protocol I,” Dr. Wells said. Protocol I found that for DME involving the central macula, intravitreal ranibizumab with prompt or deferred (24 weeks or more) focal/grid laser was more effective through 2 years in improving visual acuity than focal/grid laser treatment alone.
Five years out, he said, half of the eyes assigned to deferral of laser in Protocol I never received a laser treatment. “That knowledge has made me very slow to do laser now.” He added that 5-year follow-up showed some signs that eyes treated with ranibizumab and deferral of laser for 6 months had better long-term visual outcomes than eyes treated with ranibizumab and immediate laser.
Thus, in Protocol T, laser photocoagulation therapy for persistent edema was required, but only after 6 months of injections. Aflibercept-treated eyes were less likely to get laser than those in the other two groups. Laser was performed at least once between 24 and 48 weeks in 37% of aflibercept group, compared with 46% in the ranibizumab group and 56% in the bevacizumab group.
But don’t dismiss laser. In nonfoveal-involving edema with clearly visible extrafoveal leaking microaneurysms, focal laser may still be a good option in select patients, Dr. Ehlers said. However, for foveal-involving edema, pharmacotherapy should be considered the first-line approach, he said.
|
A Closer Look at Bevacizumab
An editorial by Martin and Maguire in the New England Journal of Medicine6 endorsed bevacizumab as first-line therapy for patients in the better vision subgroup, which, the authors noted, includes 75% of patients with DME in the general population. Given no significant differences in safety and efficacy among the drugs in the subgroup with better vision, doctors have a choice, the authors noted. And because of the price disparity among the agents, the authors made a case for choosing bevacizumab, at $50 per dose, compared with $1,200 for ranibizumab and $1,950 for aflibercept.
Anatomic findings. Yet Dr. Ho, who acknowledged that Protocol T gives ophthalmologists options, also said he reserves bevacizumab for cases in which there are no other alternatives. “The differences we saw in T tell us that bevacizumab is really an inferior choice for the treatment of DME, at least in the Protocol T study population,” he said. “Bevacizumab did not dry the macula as well, and visual acuity gains were not as strong as those noted with aflibercept and ranibizumab.”
Dr. Ehlers questioned how bevacizumab would perform over time. “These are young people, and it’s a chronic disease.” He pointed out that bevacizumab may provide VA similar to the other drugs in the better VA subgroup, but it leaves patients with a thicker retina than the other drugs do. “Over the long haul, does the eye maintain the same visual acuity? The unknown long-term implications of the residual retinal thickening may be an important variable for the durable effect of these drugs,” he said.
The bevacizumab-treated eyes on average had significantly less reduction in DME on the OCT measurement than the eyes treated with the other 2 drugs, Dr. Wells said. But this was not associated with a worse visual outcome in the eyes with better baseline vision. “Whether we will see less vision in the bevacizumab-treated eyes in year 2 remains to be seen,” he said. While acknowledging that the OCT findings could justify choosing ranibizumab over bevacizumab in the better vision group, he said, “I think you can be comfortable using Avastin and following those patients until we have data from the second year of the study.”
Safety issues. Compounding is another concern. “The bevacizumab in this study was specifically produced with quality controls that we don’t get from our usual Avastin supply chain, and we know there is variability in compounding,” Dr. Ho said. “This is important because many of the payers are forcing us to consider less expensive medications, even when they may not be in the best interest of the patient. As always, the fundamental question is, ‘What would I choose for my own family member?’”
What’s Next?
Questions remain. “We don’t know why Eylea was more beneficial than the other drugs in eyes with worse vision. This would be interesting to understand and study,” Dr. Wells said. “We also don’t know the effect of switching anti-VEGF agents. How do we manage eyes that have chronic, persistent DME, despite anti-VEGF therapy for as long as 2 years? And when do we choose steroids over anti-VEGF agents?” For now, Dr. Wells said, it’s important to know that all 3 drugs were effective. “Regardless of the drug they received, patients, on average, improved. That’s a great result, not only for us in America, but for the world. Avastin is effective.”
Dr. Ho agreed. “We have more tools available than ever before for this leading cause of adult blindness in this country. We’re really lucky,” he said. “But we can do better.” For example, new molecules that activate the TIE2 pathway are being explored, “and they may raise the bar even higher.” In addition, he said, “corticosteroids are an effective and relatively underused DME treatment option considering the totality of the data and should be considered as adjunctive or secondary therapy; they are not without side effects but these can typically be managed.”
For now, Protocol T and the other DRCR.net studies are having a profound impact on both treatment and public health. “You’re talking about getting working-age people functioning again,” Dr. Lauer said. “They can keep their driver’s licenses, their jobs, their health insurance. And they can look after their families. That’s what these treatments do. We’re getting the best outcomes we’ve ever had.”
___________________________
1 Diabetic Retinopathy Clinical Research Network. N Eng J Med. 2015;372(13):1193-1203.
2 Nguyen QD et al. Ophthalmology. 2012;119(4):789-801.
3 Massin P et al. Diabetes Care. 2010;33(11):2399-2405.
4 Korobelnik JF et al. Ophthalmology. 2014;121(11);2247-2254.
5 Diabetic Retinopathy Clinical Research Network. Ophthalmology. 2012;119(11):2312-2318.
6 Martin DF, Maguire MG. N Eng J Med. 2015;372(13):1260-1261.
Meet the Experts
JUSTIS P. EHLERS, MD Assistant professor of ophthalmology, Cole Eye Institute, Cleveland Clinic. Relevant financial disclosures: Alcon: C; Genentech: S; Regeneron: S.
ALLEN C. HO, MD Director of clinical retina research, Wills Eye Hospital, and professor of ophthalmology, Jefferson Medical College. Relevant financial disclosures: Genentech: C,S; Regeneron: C,S.
ANDREAS K. LAUER, MD The Kenneth C. Swan Professor & Vice-Chair for Education Residency Program Director, and Chief, Vitreoretinal Division, Casey Eye Institute–Oregon Health & Science University in Portland. Relevant financial disclosures: Acucela: S; Allergan: S; Applied Genetic Technologies: S; Genentech: S; National Institutes of Health (NEI, NIDDK): S; Oxford BioMedica: C,S; SanofiFovea: S.
JOHN A. WELLS III, MD Chair of ophthalmology, University of South Carolina School of Medicine, and affiliated with Palmetto Retina Center, West Columbia, S.C. Relevant financial disclosures: Genentech: S; Regeneron: S.
MARCO ZARBIN, MD, PHD, FACS The Alfonse Cinotti, MD/ Lions Eye Research Professor, and Chair, Institute of Ophthalmology & Visual Sciences, Rutgers–New Jersey Medical School, Rutgers University. Relevant financial disclosures: Calhoun Vision: C; Genentech/Roche: C; Helios KK: C; Makindus: C; Novartis: C; Ophthotech: C.
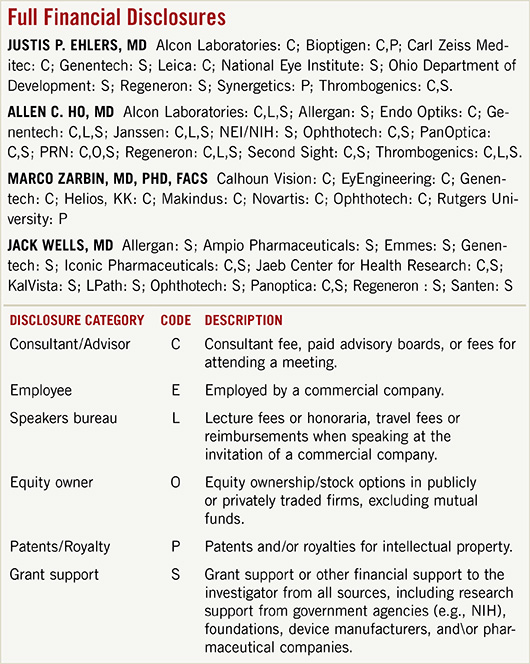
For full disclosures and the disclosure key, see below.
|