By Maram E.A. Abdalla Elsayed, MD, Yahya Al-Najmi, MD, and Hassan Mansoor, MBBS, FRCSEd, FICS
Edited By: Bennie H. Jeng, MD
Download PDF
Conjunctivitis is an inflammation of the thin, transparent, continuous mucous membrane that covers the inside of the eyelids and sclera. Most cases seen by ophthalmologists are bilateral and are most commonly caused by adenovirus. Unilateral conjunctivitis is seen less frequently, and chronic unilateral conjunctivitis is even more uncommon. (Conjunctivitis lasting longer than three weeks can be considered chronic.)
A thorough differential diagnosis for chronic unilateral conjunctivitis is vital to avoid overlooking or misdiagnosing potentially dangerous disease. In addition, it facilitates identification of easily treatable conditions that might otherwise lead to multiple unnecessary trips to the clinic—and patient frustration. The list ranges from relatively benign episodes of toxic or allergic conjunctivitis to more serious ocular and even life-threatening conditions, such as lymphoma, ocular surface neoplasms, or carotid cavernous fistula.
Differential Diagnosis
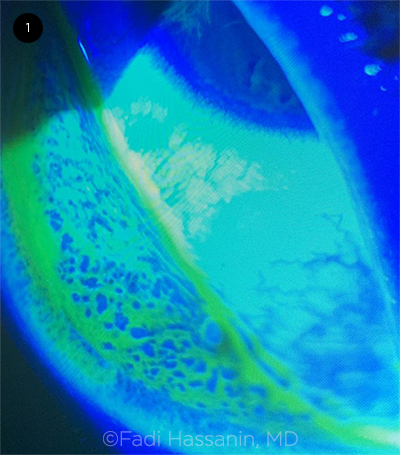
Infectious. Chlamydia trachomatis is the most frequent cause of chronic unilateral follicular conjunctivitis, but molluscum contagiosum and herpes simplex should also be taken into consideration as causative agents (Fig. 1). Subconjunctival hemorrhages, chemosis, pseudomembranes, or viral vesicles from molluscum or herpes simplex may be found concurrently and aid in the diagnosis.
Parinaud oculoglandular syndrome is a rare, chronic, unilateral granulomatous conjunctivitis accompanied by adjacent preauricular lymphadenopathy that may be suppurative. Causes of this syndrome include cat-scratch disease, tuberculosis, atypical mycobacteria, and syphilis.
Inflammatory and autoimmune. Keratoconjunctivitis sicca–causing disease, such as sarcoidosis, rheumatoid arthritis, and systemic lupus erythematosus (SLE), may present as unilateral conjunctivitis. Sarcoidosis may also cause a follicular conjunctivitis without keratoconjunctivitis sicca.1
Masquerade syndrome. Sebaceous neoplasia of the meibomian gland, Zeiss gland, or both may present as a chronic unilateral conjunctivitis. Squamous conjunctival carcinoma classically occurs on the bulbar conjunctiva, originating at the limbus, and may often spread into the cornea. Primary ocular lymphoma and other intraocular malignancies may also masquerade as chronic conjunctivitis.
 |
|
CONJUNCTIVAL STAINING. Slit-lamp examination with fluorescein staining of an eye with viral follicular conjunctivitis.
|
History
Asking the right questions in the history is crucial for early and accurate diagnosis. Following are examples of queries to uncover diagnostic clues.
Was there exposure to any ocular medications? Did any facial creams, ointments, cosmetics, or hairspray get in the eye area? Any of these preparations could be responsible for an atopic conjunctival reaction. Topical medications, such as atropine, scopolamine, antibiotic eyedrops (e.g., gentamicin, neomycin, sulfonamides, amphotericin B), topical antiviral medications (e.g., trifluridine, vidarabine, idoxuridine), glaucoma medications (e.g., pilocarpine, apraclonidine, latanoprost), and lubricating eyedrops containing benzalkonium chloride, can induce a follicular conjunctival response, mainly involving the inferior conjunctiva.
Is there a history of contact lens wear, ocular prosthesis, or ocular surgery with a possibility of exposed sutures? These may cause a unilateral giant papillary conjunctivitis (Fig. 2) and a diffuse corneal staining pattern.
Is there a history of systemic disease? Autoimmune disease, such as rheumatoid arthritis and SLE, may cause keratoconjunctivitis sicca, as can lacrimal gland infiltration in sarcoidosis. Superior limbic keratoconjunctivitis in particular is associated with thyroid dysfunction, whether hyperthyroidism, hypothyroidism, or euthyroid Graves disease.
Is there a history of other conditions that could cause nasolacrimal duct (NLD) obstruction? Previous sinus disease, trauma, ocular or nasal surgery, chemotherapy, and treatment with radiation or radioactive iodine can result in secondary NLD obstruction and associated unilateral conjunctivitis.
Is there a family history of spondyloarthropathies or inflammatory back pain? The presence of these symptoms should prompt further questioning regarding extraspinal features of spondyloarthritis, such as inflammatory bowel disease, psoriasis, dactylitis, and enthesitis (particularly of the heel).2
Was there exposure to cats or rabbits? The bacteria Bartonella henselae and Francisella tularensis are endemic in cats and rabbits, respectively, and cat-scratch disease is the most common cause of Parinaud oculoglandular syndrome.
 |
|
PAPILLAE. Papillary conjunctivitis in the tarsal conjunctiva caused by chronic contact lens use.
|
Examination
During an external eye exam for conjunctivitis, the patient should be asked to look up and down, and the eyelids should be everted.
Face and eyelids. The periocular skin and the rest of the face should be carefully examined, including the eyelid margins, eyelashes (madarosis may suggest chronic lid pathology), and the medial canthus (the “pouting punctum” of canaliculitis may be overlooked and should be carefully compared to the contralateral puncti).
Molluscum. In children, the characteristic centrally umbilicated, pearly papules of molluscum may be distributed extensively, sometimes beyond the face to the trunk, limbs, and axillary areas.
Carotid cavernous fistula. Even a suspected proptosis should be noted, as patients with a low-flow carotid cavernous fistula can present with “chronic conjunctivitis” recalcitrant to medical therapy.3
Eyelid laxity. An easily everted, hyperelastic lid may point to floppy eyelid syndrome.
Foreign bodies. When unilateral keratoconjunctivitis is seen in a young child, the clinician should be alert to the possibility of an occult foreign body under the lids. Although foreign bodies are usually cleared from the ocular surface by the blink reflex and reflex tearing, they are occasionally retained and become encapsulated by mucus and a local inflammatory reaction.4 Chronically retained foreign bodies may present with abrasions or even keratitis caused by the exotoxins released by bacterial flora surrounding the foreign body.4
Medial canthus. The clinician should palpate the lacrimal sac, watching for any swelling, tenderness, or reflux. Tearing and matted eyelashes may be present in chronic dacryocystitis (Fig. 3); however, some patients may show no signs of acute inflammation and may recount only a history of chronic sinus disease or facial trauma.5 Elderly women, in particular, may suffer from progressive essential dacryostenosis.
Lymph nodes. The preauricular and submandibular lymph nodes should be palpated. Enlargement of the nodes may indicate viral or chlamydial etiologies or Parinaud oculoglandular syndrome.
Fornix. A deeper-than-normal superior conjunctival fornix associated with senile upper lid ptosis and a mucopurulent coagulum in the upper fornix recesses may indicate giant fornix syndrome.
A larger-than-normal tear meniscus and prolonged retention of fluorescein dye may suggest lacrimal duct obstruction.
Conjunctiva and cornea. Particular attention should be focused on conjunctival scarring, corneal opacities, and the shape and size of the pupil. These features may point to an infectious, inflammatory, or uveitic cause.
Uveitis. HLA-B27–associated conjunctivitis or acute anterior uveitis occurs most commonly in young adult patients. Even though the cause is unknown, possible triggers include infection with C. trachomatis, Enterobacter, Shigella, Salmonella, or Campylobacter. In HLA-B27–positive children, Yersinia infections may incite conjunctivitis.6
Neoplasia. Papillary hypertrophy of the palpebral conjunctiva may warrant biopsy to rule out neoplasia, even when there is no sign of an underlying chalazion-like eyelid mass, as some patients have chronic unilateral blepharoconjunctivitis before the tumor is clinically apparent. Sebaceous gland carcinoma may spread through the conjunctiva in a pagetoid manner and, more commonly, involve the superior lid, where meibomian and Zeiss glands are more numerous.
Mucus fishing syndrome. Conjunctival staining in the inferonasal quadrant of the bulbar conjunctiva in patients with chronic ocular surface inflammation of any cause may indicate mucus fishing behavior. The inferonasal quadrant is involved because of its accessibility. These patients admit to the underlying problem. However, this remains a diagnosis of exclusion.
 |
|
DACRYOCYSTITIS. Right eye of woman with dacryocystitis, with matting of eyelashes, tearing, and crusting.
|
Other Diagnostic Studies
Diagnostic workup for atypical case presentations may include blood tests to rule out systemic infections, inflammations, endocrine dysfunctions, and oncologic etiologies. Imaging may be necessary to assess for orbital involvement or retro-orbital pathologies. X-rays of the chest as well as lumbar and thoracic spine may be required if sarcoidosis or a spondyloarthropathy is suspected.
Management
Treatment of chronic unilateral conjunctivitis depends on accurate diagnosis of the cause. In case of underlying systemic conditions, consultation and coordination are needed between the ophthalmologist and the patient’s primary care physician or other medical specialists.
Infectious causes. Chlamydial conjunctivitis can be treated with doxycycline 100 mg twice a day for 10 days or a single dose of azithromycin 1 g. Erythromycin is a safer option for pregnant women and for infants. (Infant dosing is 50 mg/kg/day in four divided doses daily for two weeks.)
Molluscum contagiosum lesions must either be treated by cryotherapy or excised and cauterized at the base.
Treatment for patients with Parinaud oculoglandular syndrome is mainly supportive. However, severe cases require oral antibiotics, the selection of which depends on the specific infectious agent.
Inflammatory and autoimmune conditions. Patients need to be examined for underlying systemic causes and should be treated in coordination with a rheumatologist. Ocular symptoms can be managed with preservative-free lubricant eyedrops and ointments at bedtime, as well as topical steroids for short-term use when necessary.
Masquerade syndromes and neoplasia. These lesions must be biopsied, and subsequent management depends on the histopathologic type, disease stage, and specific demands of the patient.
Toxic or mechanical causes. The offending agent should be identified and discontinued if possible. If the cause is an ocular medication, the patient should be switched to an unpreserved formulation of the same drug, if available. However, the pros and cons of discontinuing a medication should be weighed carefully, as the consequences of stopping may be more serious than the iatrogenic conjunctivitis.
Loose or exposed sutures that cause irritation should be removed. Contact lens wearers may be advised to replace soft contact lenses more frequently or replace rigid contact lenses.
NLD obstruction. When NLD obstruction is present, an oculoplastic or otolaryngology referral may be needed for possible external or endoscopic dacryocystorhinostomy.
Conclusion
Chronic unilateral conjunctivitis is a relatively rare entity, and accurate and timely identification of its underlying cause can substantially reduce morbidity and clinical visits. Diagnosis is based on a thorough history and careful examination to assess the morphology and localization of the disease process, after which appropriate treatment can be commenced.
__________________________
1 Papadaki TG et al. Ocul Immunol Inflamm. 2006;14(5):309-311.
2 Weisman MH. Rheum Dis Clin North Am. 2012;38(3):501-512.
3 Alam MS et al. Sci Rep. 2019;9(1):12872.
4 Babu K, Maralihalli RE. Indian J Ophthalmol. 2009;57(6):473-474.
5 Yakopson VS et al. Saudi J. Ophthalmol. 2010;25:37-49.
6 Saari KM et al. Int Ophthalmol. 1986;9(4):237-241.
__________________________
Dr. Elsayed is an ophthalmology specialist at Jeddah Eye Hospital and Dr. Al-Najmi is an ophthalmology specialist at Saggaf Eye Centre; both are in Jeddah, Saudi Arabia. Dr. Mansoor is cornea and external eye disease consultant at Al Shifa Trust Eye Hospital, Rawalpindi, Pakistan. Financial disclosures: None.