By Michael P. Mott, Contributing Writer, interviewing Ahmad A. Aref, MD, Augusto Azuara-Blanco, PhD, and Steven J. Gedde, MD
Download PDF
The prevalence of primary angle-closure glaucoma (PACG) is growing at a substantial rate. By 2020, it will affect 23 million people worldwide between the ages of 40 and 80. By 2040, that number will jump to 32 million.1 And although primary open-angle glaucoma is more common, PACG is more severe and more likely to cause irreversible blindness, making early and effective treatment critical.
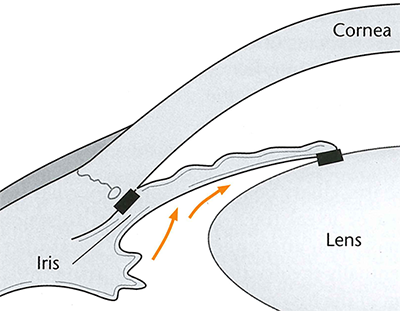
Traditionally, the standard of care for PACG and the early stage of the disease—primary angle closure (PAC)—has been laser peripheral iridotomy to open the drainage pathways along with eyedrops to reduce intraocular pressure (IOP). Because the lens plays an important role in the pathogenesis of the disease, an alternative approach—surgical lens extraction—has also been used to treat patients who have a coexisting cataract.
But should ophthalmologists consider removing a perfectly healthy lens to treat this type of glaucoma? Findings from a landmark clinical trial show that, for certain patients, not only is clear lens extraction safe and efficacious, but it also should be considered a first-line treatment.2
The EAGLE Study
For the Effectiveness inAngle-Closure Glaucoma of Lens Extraction (EAGLE) study, Augusto Azuara-Blanco, PhD, at Queen’s University Belfast, Northern Ireland, and other investigators from the United Kingdom and the United States conducted a randomized controlled trial that included 155 patients with PAC and 263 with PACG from 30 clinics across 5 countries. The researchers assessed the efficacy, safety, and cost-effectiveness of clear lens extraction versus laser peripheral iridotomy for the first-line treatment of PACG and PAC.
Inclusion criteria for patients were:
- age 50 years or older,
- absence of cataract, and
- mild or moderate PACG or newly diagnosed PAC with IOP of 30 mm Hg or greater.
Clinical results. Of the 419 patients included, 208 underwent clear lens extraction and 211 standard care with laser iridotomy. Thirty-six months after treatment, the results showed what Dr. Azuara-Blanco and his team considered to be an unquestionable advantage of lens extraction for all outcome measures. In particular:
- Mean IOP was 1.18 mm Hg lower in the lens extraction group.
- Mean self-reported health status, as measured by the European Quality of Life–5 Dimensions questionnaire and other measures of vision-related quality of life, was higher in the lens extraction group.
The economics. Clear lens extraction was also more cost-effective. The initial costs were higher compared with standard care, but these were offset by fewer subsequent procedures and a less burdensome medication regimen. And in a separate economic evaluation of the EAGLE trial, Dr. Azuara-Blanco and investigators found that lens extraction might actually serve as a cost-saving strategy after the course of 10 years.3
Based on these results, he noted, “there is now robust evidence that clear lens extraction is associated with better clinical and patient-reported outcomes than the traditional standard of care.” Moreover, for the specific segment of patients included in the trial, laser peripheral iridotomy as the initial treatment for angle-closure glaucoma should be reconsidered.
 |
|
PACG. For primary angle-closure glaucoma, clear lens extraction may confer some advantages over iridotomy.
|
Findings a Surprise
For Ahmad A. Aref, MD, at the University of Illinois Eye and Ear Infirmary in Chicago, these results were a bit of a shock. “Before the results were published, I didn’t expect there to be much of a difference between the two treatment groups,” he said. “My personal preference has always been to first proceed with laser iridotomy in almost all cases of PAC without cataract, and I never gave much thought to clear lens extraction as the initial treatment. So I was very surprised to find that the extraction of a healthy lens was more beneficial in every major outcome variable.”
Dr. Aref found it particularly interesting that patients randomized to lens extraction required fewer surgical procedures and glaucoma medications after 3 years of follow-up. “That is the most powerful finding and their most powerful argument for clear lens extraction,” he said, “particularly because incisional glaucoma surgery carries with it more risk.”
These results matter, added Dr. Aref, because they have implications for every glaucoma physician. “The EAGLE study is a breakthrough because it challenges the very standard of care for this segment of patients with PAC and PACG,” he said. “Currently, it is highly unusual for a clinician to recommend removing a lens as first-line treatment if the patient has no cataracts—it probably occurs in less than 10% of cases. But these researchers are showing that we need to rethink a practice guideline that’s very well-ingrained in our field.”
Incorporation Into Practice
Will physicians actually recommend the option of removing a healthy lens to their PAC and PACG patients?
Steven J. Gedde, MD, at the Bascom Palmer Eye Institute in Miami, is convinced that they will. “This landmark trial has the potential to produce a real paradigm shift in how we manage a specific type of patient, namely those with PACG or PAC with significantly elevated IOP. It is certainly information that I will share with patients of this type, and it will likely influence my decision to proceed with lens extraction earlier in the course of management.”
Dr. Aref agreed, “I do think this will eventually become mainstream practice. Given these published findings, it really is now the ophthalmologist’s duty to mention the option of clear lens extraction. For patients with similar characteristics to the patients included in this study, it would be very difficult for me not to at least mention the procedure as an option.”
Reservations. Dr. Aref does expect a few of his colleagues to remain apprehensive about the study’s recommendations. For some, the extraction of the lens is so synonymous with cataract surgery that they might have difficulty with converting the EAGLE results to practice. For others, there will always be a concern with the loss of accommodation associated with an artificial lens.
Slow uptake. Dr. Gedde pointed out that no one should expect practice patterns to change immediately. “Randomized clinical trials like this one represent the highest level of evidence-based medicine for guiding patient care. But past experience has shown us that it takes many years to translate trial results into clinical practice.”
Patient Selection Critical
Because a majority of patients with PAC present with an IOP well under the 30 mm Hg threshold used in the EAGLE study, ophthalmologists may wonder if these findings apply to the broader spectrum of cases that they see on a day-to-day basis. According to Dr. Azuara-Blanco, the answer is no.
He is adamant that people avoid extrapolating these results to patients outside of the study’s entry criteria. “Colleagues have expressed some concern that clinicians may misinterpret or perhaps misuse the results of the EAGLE trial. We don’t want to generalize our findings to patients who have, say, narrow angles or angle-closure glaucoma with advanced damage. The key point is that the trial doesn’t say that you must perform clear lens extraction—it’s simply validating another treatment option to discuss with your patients.”
Dr. Gedde agreed. “The EAGLE study looked at a very specific population. Ophthalmologists should be very cautious about applying the results of this study to dissimilar patient groups.”
Additional Questions
The EAGLE results are certainly intriguing; however, a few questions remain. As Dr. Gedde points out, 9% of the patients in the study underwent goniosynechialysis at the surgeon’s discretion in combination with lens extraction. “But this combined procedure is different than lens extraction alone,” he said. “Was there a difference in outcome in this subgroup?” He also noted that the researchers did not report the degree of appositional and synechial angle closure in most patients, which was likely an important prognostic indicator. In addition, the patient and investigator were not masked to the randomized treatment assignment, thus creating a potential source of bias.
Nonetheless, Dr. Gedde and Dr. Aref noted that this trial will surely open up exciting new avenues of investigation. “This study could have a particularly important impact in areas like Asia, specifically east Asia, where PACG is the predominant form of glaucoma, as well as other areas where health care resources are limited,” said Dr. Aref. “And so these EAGLE results can really help inform a look at how different subgroups and different ethnicities will respond to clear lens extraction compared with a variety of interventions.”
In fact, such studies are underway. According to Dr. Azuara-Blanco, his colleague David S. Friedman, MD, MPH, PhD, a U.S. ophthalmologist on the EAGLE team, is already conducting a clinical trial similar to EAGLE in China.
___________________________
1 Tham YC, et al. Ophthalmology. 2014;121(11):2081-2090.
2 Azuara-Blanco et al. Lancet. 2016;388(10052):1389-1397.
3 Javanbakht M et al. Br Med J Open. 2017;6:e013254. doi:10.1136/bmjopen-2016-013254.
___________________________
Dr. Aref is associate professor of ophthalmology, Glaucoma Service, and director of the Residency Training Program, Illinois Eye and Ear Infirmary, University of Illinois College of Medicine, Chicago. Relevant financial disclosures: None.
Dr. Azuara-Blanco is professor of ophthalmology at the School of Medicine, Dentistry, and Biomedical Sciences, Queen’s University Belfast in Northern Ireland. Relevant financial disclosures: None.
Dr. Gedde is professor of ophthalmology and vice chair of education at the Bascom Palmer Eye Institute in Miami. Relevant financial disclosures: None.
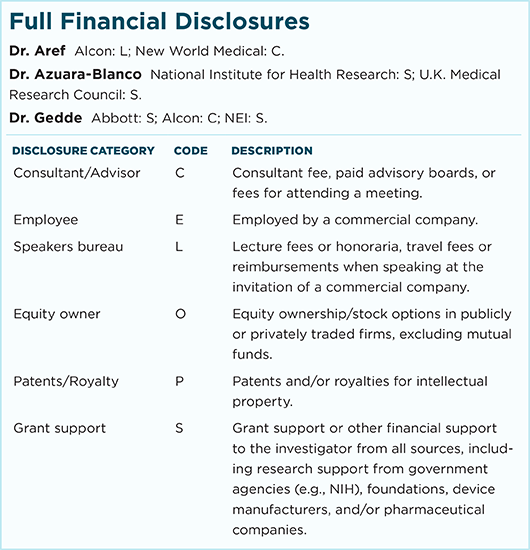
For full disclosures and the disclosure key, see below.