By William A. Pearce, MD, Parker J. Williams, BS, Jill R. Wells, MD, and Jiong Yan, MD
Edited by Steven J. Gedde, MD
Download PDF
Did Becky Jones* have age-related macular degeneration (AMD)? Her ophthalmologist certainly thought she might, which is why she was referred to our university retina service.
Six months before we saw Ms. Jones, the 71-year-old woman underwent bilateral uncomplicated cataract surgery and had a multifocal intraocular lens (IOL) implanted in each eye. Two months later, she suddenly began to experience nyctalopia. Over the next 4 months, her vision continued to gradually and painlessly decline. At that point, she was referred for evaluation of what appeared to be AMD.
We Get a Look
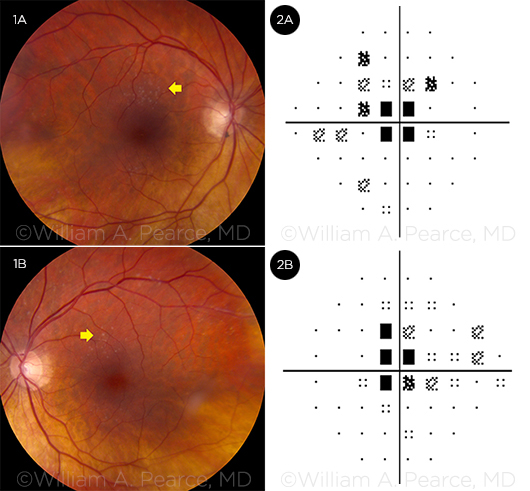
When we examined Ms. Jones, her best-corrected visual acuity was 20/50 in her right eye and 20/60 in her left. Her intraocular pressure (IOP) was normal in both eyes, and there was no afferent pupillary defect. The anterior segment examination revealed well-positioned multifocal IOLs. The posterior segment exam revealed clear vitreous, pink and sharply defined discs, mildly attenuated arterioles, and deep granular white deposits at the level of the retinal pigment epithelium (RPE) in the macula (Figs. 1A, 1B).
 |
|
WHAT’S YOUR DIAGNOSIS? (Figs. 1A, 1B) The posterior segment exam revealed deep granular white deposits at the level of the RPE in the macula (arrows). (Figs. 2A, 2B) Additional testing with Humphrey visual fields showed bilateral centrocecal scotomas.
|
Digging Deeper
At this point, we had a patient with a presumptive diagnosis of AMD but whose macular lesions did not have the classic appearance of drusen. Furthermore, her symptoms were rather abrupt in onset and fairly dramatic in severity. This led us to probe further into her medical history.
It turned out that Ms. Jones had been diagnosed with ovarian cancer as a young woman. The cancer was treated with oophorectomy and extensive abdominal radiation.
Subsequently, she had experienced chronic complications from intestinal adhesions, including a small-bowel obstruction that had required resection. The resection was performed some 10 years before we saw her, and after this surgery, she was left with approximately 100 cm of small bowel and suffered from chronic diarrhea.
Pinning It Down
This additional information led us to broaden our search.
Differential diagnosis. Because of Ms. Jones’ history of ovarian cancer, we were concerned that she might have cancer-associated retinopathy. Given her chronic diarrhea in the setting of intestinal resection, we were also worried about the possibility of fat-soluble vitamin deficiency.
Additionally, we considered the possibility of nyctalopia induced by her multifocal IOLs.
Office-based diagnostics. At this point, we ordered a series of tests. Humphrey visual fields demonstrated a central scotoma with a preserved peripheral field in both eyes, suggesting macular disease (Figs. 2A, 2B). Electroretinography revealed moderate rod-cone dysfunction, confirming an intrinsic problem in the retina.
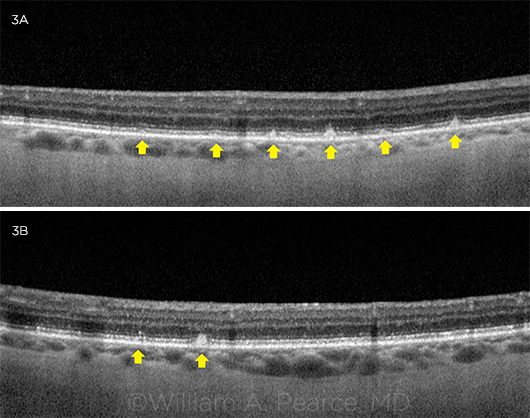
Spectral-domain optical coherence tomography (SD-OCT) showed focal areas of disruption in the ellipsoid zone as well as retinal granular deposits (Figs. 3A, 3B). Fundus autofluorescence imaging displayed a stippled hypoautofluorescence pattern corresponding to the white deposits seen on the clinical examination.
 |
|
PINNING IT DOWN. (Figs. 3A, 3B) SD-OCT scans showed focal areas of disruption in the ellipsoid zone as well as the granular deposits (arrows).
|
A Definitive Answer
Following this evaluation, we hypothesized that Ms. Jones had a fat-soluble vitamin deficiency. She was sent immediately to our laboratory, where serum analysis revealed retinol (vitamin A) levels less than 0.06 mg/L and a retinyl palmitate level less than 0.02 mg/L, indicating a severe vitamin A deficiency. (In our lab, a retinol level greater than 0.3 mg/L is within normal range and a level less than 0.10 mg/L is indicative of a severe deficiency.)
A diagnosis of vitamin A deficiency retinopathy was made, and Ms. Jones was started on a high-dose oral formulation of vitamin A.
Discussion
Vitamin A is an essential micronutrient that is vital to retinal functioning, epithelial development, and immune health. Its absorption is concurrent with fats in the latter third of the small intestine. Once absorbed, predominantly as retinyl esters via chylomicrons and retinol via the portal system,1 vitamin A derivatives are converted into biologically active forms, most notably 11-cis-retinol in photoreceptors and retinoic acid in epithelial tissue. Trans-retinol is oxidized into 11-cis-retinol in the RPE, and this action is essential for the formation of the photopigment rhodopsin in the rods and cones. Retinoid metabolism is a critical process that occurs between the pigment epithelium and neural retina and allows for recycling of essential photopigments.
Deficiency of vitamin A is a well-documented international problem, predominantly due to malnourishment in children and pregnant women.2 Conventional wisdom holds that vitamin A deficiency is uncommon in developed nations, but the experience at our center has demonstrated an increasing prevalence of this condition in patients with a history of intestinal disease.
Our case exemplifies many of the classic findings of this increasingly common condition. The deep retinal granules do not have the classic yellow appearance of drusen found in AMD, and the distribution is typically outside of the macula. The histochemical composition of these deep retinal granules has not been elucidated, but they are classically present around the arcades and in the nasal retina. The distribution and appearance of these lesions should steer the clinician away from a diagnosis of AMD. Moreover, ancillary testing helps reveal an absence of typical drusen under the RPE.
Other Considerations
Patients with multifocal IOLs are known to have near vision problems under mesopic conditions, predominantly related to pupillary dilation in a low light setting. However, a careful history will confirm that the nyctalopia of vitamin A deficiency retinopathy occurs at all distances and in low light conditions.
Additionally, cancer-associated retinopathy is a spectrum of paraneoplastic disorders in which the presence of antibodies to retinal proteins causes a progressive decline in photoreceptor function. This presentation may occur in the setting of a known malignancy, but in the absence of other clues it should stimulate a systemic evaluation.
In our case, the classic retinal findings of vitamin A deficiency and remote history of treated malignancy reduced the likelihood of a diagnosis of cancer-associated retinopathy; nonetheless, we obtained an antiretinal antibody panel to exclude the possibility of this rare disease.
___________________________
* Patient name is fictitious.
___________________________
1 Harrison EH. Ann Rev Nutr. 2005;25:87-103.
2 World Health Organization. Global Prevalence of Vitamin A Deficiency in Populations at Risk 1995-2005. WHO Global Database on Vitamin A Deficiency. Accessed Dec. 9, 2016.
___________________________
Dr. Pearce is a vitreoretinal surgery fellow, Mr. Williams is a premedical student, Dr. Wells is a comprehensive ophthalmologist and ocular oncologist, and Dr. Yan is a retina specialist and director of the vitreoretinal surgery fellowship; all are at the Emory University Eye Center in Atlanta. Relevant financial disclosures: None.