By Courtney Y. Kauh, MD, MS, and Christine C. Nelson, MD, FACS
Edited by Sharon Fekrat, MD, and Ingrid U. Scott, MD, MPH
Download PDF
Mucormycosis is an aggressive opportunistic fungal infection, also known as phycomycosis and zygomycosis. Although mucormycosis can affect other parts of the body such as the lungs and gastrointestinal tract, this review focuses on the rhinocerebral-orbital type. It is caused by organisms of the family Mucoraceae (including the genera Mucor, Absidia, and Rhizopus).1
The fungus that causes the disease is ubiquitous in nature and is found in soil and on decaying vegetation. Because the fungus is so widespread, humans are exposed to it on a regular basis. The spores of the fungus are inhaled through the mouth and nose, but infection rarely occurs in a person with an intact immune system because macrophages phagocytize the spores. However, an immunocompromised individual is unable to mount an effective immune response against the inhaled spores; thus, germination and hyphae formation occur and infection develops, most commonly in the sinuses and lungs.
When the fungus invades the paranasal sinus mucosa, it may spread directly to the orbital apex and, from there, gain intracerebral access. Mucormycosis is difficult to diagnose early, as patients often present with nonspecific symptoms. By the time signs of orbital apex involvement develop, it is often too late to save the patient’s vision, or even the patient’s eye or life. The presentation is typically a rapidly progressive infection, and the disease is associated with a high mortality rate.
Orbital Imaging. (1A) CT of the orbits shows opacification of the right paranasal sinus. (1B) MRI demonstrates correlating nonenhancement of the right nasal sinus mucosa.
Epidemiology
The disease has a predilection for distinct patient populations. These include individuals with diabetes mellitus (especially those with diabetic ketoacidosis); persons who have received multiple blood transfusions; immunocompromised patients with severe neutropenia such as those with transplants or hematopoietic malignancies; or those on chronic steroids or immunosuppressants.2,3
Pathogenesis
Diabetic or immunocompromised patients most commonly present with sinus disease. The organisms often invade the paranasal sinus mucosa; they may remain contained there or progress into the orbit or brain parenchyma, causing sino-orbital and/or rhinocerebral infections, respectively.3 The fungal hyphae directly invade blood vessels, producing tissue infarction and massive necrosis with bone destruction.4-6
The ethmoid sinus is an important route of infection, since mucormycosis may invade through the thin lamina papyracea and gain access to the orbit and its contents. From here, the organisms may extend posteriorly to the orbital apex, leading to orbital apex syndrome. The optic nerve may be affected, resulting in vision loss. Involvement of the superior orbital fissure and its contents, such as cranial nerves III, IV, and VI, and branches of V1 and V2, may cause diplopia, ophthalmoplegia, and sensory loss to the corresponding areas of the cornea and face. With further posterior extension, the fungus may gain access to the cavernous sinus and to the brain parenchyma, causing vascular thrombosis and infarction. Mucormycosis is aggressively invasive, and thus, progression of the infection may be very rapid.
Presentation
The onset of sinus mucormycosis may be associated with nonspecific symptoms such as nasal congestion, postnasal drip, dark blood-tinged or purulent rhinorrhea, sinus tenderness, headache, fever, and malaise. Because the condition may lead to angioinvasion and tissue infarction, infection of the ethmoid sinus may penetrate through bone and soft tissue and cause an eschar to form over the infected area. A black necrotic eschar on the nasal turbinates or hard palate is characteristic of maxillary sinus involvement.
As the infection progresses, late symptoms may include facial or periorbital swelling or numbness, blurred vision, chemosis, proptosis, diplopia, ophthalmoplegia, corneal anesthesia, and loss of vision, which are indicative of invasion of the orbital nerves and vessels. The occurrence of mental status changes, hemiparesis, or seizures suggests intracranial invasion.6 The time from onset of initial symptoms to late symptoms and signs that are diagnostic of the disease may be as short as one day.7 The development of late symptoms and signs indicates a poor prognosis.
Diagnosis
Imaging. With sinus involvement, magnetic resonance imaging (MRI) may demonstrate variable T1 and T2 intensity with focal lack of enhancement in areas of devitalized sinus mucosa (Fig. 1). With involvement of the cavernous sinus, contrast-enhanced computed tomography (CT) scans may show lack of enhancement in this region, which is consistent with thrombosis from the invasive fungus. Other radiographic findings of mucormycosis include a rim of soft tissue thickness along the paranasal sinuses, opacification of the sinuses, fluid levels in the sinuses, and bone destruction. Because these are often nonspecific findings, it may be difficult to distinguish mucormycosis from other sinoorbital conditions.8 However, once the diagnosis of mucormycosis has been made, CT and MRI can help to delineate the extent of infection and can guide surgical debridement.
Biopsy. The signs, symptoms, and radiographic findings of mucormycosis are nonspecific; direct histologic examination of scrapings or biopsies of involved tissue or paranasal sinus secretions are diagnostic. The fungal invasion may be patchy, so multiple biopsies may be required for definitive diagnosis. Biopsy may need to be repeated if initial biopsies are negative, yet the patient has signs of progressive orbital involvement and imaging reveals affected sinuses.7
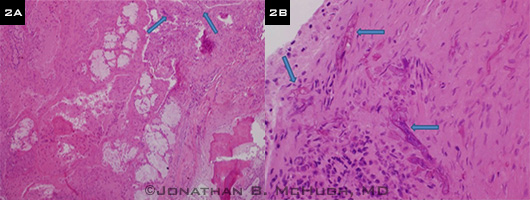
Histopathology with special stains—such as Grocott-Gomori methenamine–silver nitrate, periodic acid–Schiff, or calcofluor white—demonstrates the pathognomonic broad, irregular, nonseptate, and right-angle branching hyphae (Fig. 2). Evidence of angioinvasion and tissue infarction may also be observed.1
 |
|
Histopathology. (2A) Low-power view of fungal sinusitis with extensive tissue necrosis in the absence of a strong inflammatory response. Rare Mucor organisms (arrows) can be seen invading tissue adjacent to areas of necrosis. (2B) Mucorales organisms can be seen invading connective tissue (arrows). Typical hyphae forms are broad with irregular, thin, nonparallel cell walls lacking septae.
|
Treatment
Medical. Optimal medical therapy relies on rapid correction of underlying systemic abnormalities, such as acidemia and hyperglycemia, along with prompt antifungal initiation and aggressive surgical intervention.
Lipid-based amphotericin B, which destroys the cell wall of the fungus, is the first-line medical treatment for mucormycosis and should be initiated as soon as the diagnosis is suspected. High doses are required, and nephrotoxicity may result; however, liposomal formulations may deliver high doses while protecting renal function.
Posaconazole, a triazole that inhibits growth of the fungus, has been proposed as a promising adjunctive or alternative treatment for mucormycosis.6,9 Further studies are needed to better understand the role of posaconazole in the primary treatment of mucormycosis. Thus, at this time, it is not recommended as a first-line therapy.
Because systemic medications are often unable to reach the infected tissue due to vaso-occlusion, surgery should be considered early in the course of treatment.
Surgical. Early aggressive surgical debridement is important for successful management of invasive fungal disease. This can be done endoscopically or through an open approach. The goal is to remove all necrotic tissue. Involved tissues rarely bleed, so the surgeon should debride until normal, well-perfused, bleeding tissue is encountered. Daily repeat debridement may be needed until clinical improvement is established. With extensive spread of the disease, orbital exenteration, along with removal of the sinuses, may be necessary.
Prognosis
Before the advent of amphotericin B, mortality rates associated with mucormycosis were as high as 90 percent. The disease continues to have high mortality rates, with one study reporting a range of 50 to 80 percent.1 Another study reviewed 929 mucormycosis cases (referred to as zygomycosis in the article) and found the survival rate to be 61 percent in cases treated only with amphotericin B, 57 percent in those treated only with surgery, and 70 percent in those treated with both surgery and amphotericin B.3
Other Key Points
Because mucormyocosis may involve the orbit and other ocular structures, the ophthalmologist may be the first physician to see a patient with this highly morbid condition. Thus, it is important to have this disease in the differential diagnosis, as a delay in diagnosis may be fatal.
Aggressive medical and surgical management is critical, and patients will likely require comanagement with multiple services. Excellent communication among these services and an in-depth discussion with the family regarding prognosis are fundamental in caring for these patients.
___________________________
1 Ribes JA et al. Clin Microbiol Rev. 2000;13(2):236-301.
2 Kasapoglu F et al. Otolaryngol Head Neck Surg. 2010;143(5):614-620.
3 Roden MM et al. Clin Infect Dis. 2005;41(5):634-653.
4 Greenberg RN et al. Curr Opin Infect Dis. 2004;17(6):517-525.
5 Yohai RA et al. Surv Ophthalmol. 1994;39(1):3-22.
6 Gamaletsou MN et al. Curr Infect Dis Rep. 2012;14(4):423-434
7 Thurtell MJ et al. Clin Experiment Ophthalmol. 2013;41(6):567-576.
8 Safder S et al. AJNR Am J Neuroradiol. 2010;31(4):771-774.
9 Vehreschild JJ et al. Crit Rev Microbiol. 2013;39(3):310-324.
Dr. Kauh is a resident in ophthalmology and visual sciences, and Dr. Nelson is Bartley R. Frueh, M.D., and Frueh Family Collegiate Professor in Eye Plastics and Orbital Surgery; both are at the University of Michigan Kellogg Eye Center. The authors report no related financial interests.