By Annie Stuart, Contributing Writer, interviewing Gaurav K. Shah, MD, Rishi Singh, MD, and Charles C. Wykoff, MD, PhD
Download PDF
Retina specialists have long needed more reliable biomarkers for predicting a patient’s future vision, said Charles C. Wykoff, MD, PhD. Dr. Wykoff, in practice in Houston, added that central retinal thickness (CRT) is an imperfect predictor of outcomes for patients with diabetic macular edema (DME). “Some thick retinas see well and, conversely, some thin retinas with no macular edema see poorly.”1
Cementing this impression, Rishi Singh, MD, at the Cole Eye Institute, Cleveland Clinic, and his colleagues recently studied 900 patients, finding no correlation between CRT and visual acuity (VA). Researchers have also performed genetic, serum, and vitreous fluid analyses, he said, but these haven’t revealed associations with visual outcomes.
However, Jennifer K. Sun, MD, PhD, and her colleagues at the Joslin Diabetes Center in Boston have found that, among a variety of variables—including intraretinal cysts, microaneurysms, subretinal fluid, and external limiting membrane disruption—a change in disorganization of the retinal inner layers (DRIL) is most consistently correlated with VA.2,3 DRIL affecting at least 50% of the 1-mm central retinal zone was associated with worse VA in all eyes with current or resolved edema.
Eyes with persistent DRIL did not do well, said Gaurav K. Shah, MD, in practice in St. Louis, Missouri, and vision improved in eyes where DRIL resolved. Dr. Sun and her fellow researchers found that when DRIL decreased by 250 μm or more at 4 months, nearly 78% of eyes had VA improvement of at least 1 line.2 DRIL is a robust biomarker, although the correlation is not perfect. There are patients with DRIL who do well visually and those who don’t, said Dr. Wykoff.
The take-home message? “Don’t just look at thickness,” said Dr. Shah, “also look at morphology.”
What Is DRIL?
DRIL stands for disorganization of retinal inner layers and is the horizontal extent in microns for which the boundaries between the ganglion cell, inner plexiform, and outer nuclear plexiform layers cannot be identified, said Dr. Shah.
“Similar to the transmission of electricity through poles and wiring, the retinal inner layers transmit visual messages through neurons,” he said, “but disorganization of those layers can destroy its bipolar, amacrine, and horizontal cells, leading to poor visual outcomes.”
An SD-OCT finding. DRIL is a finding of spectral-domain optical coherence tomography (SD-OCT), said Dr. Wykoff. “If you look at the central part of the macula and can clearly visually or manually segment the inner retinal layer boundaries, then there is no DRIL,” he said. “If you cannot visualize those boundaries, then there is disorganization of the inner retinal layers, which correlates strongly with a worse prognosis if the region involves a substantial portion of the central macula.”
What causes DRIL? Although it is not universally seen across all patient groups, DRIL occurs in patients with a variety of retinal vascular diseases such as diabetic macular edema (DME) and retinal vein occlusion (RVO), said Dr. Singh. The causes of DRIL are not fully understood, added Dr. Wykoff; however, the breakdown of barriers and cellular integrity is likely a consequence of the pathology of the disease itself, such as diabetic retinopathy.
Increased risks. Chronicity appears to be key in development of DRIL.2 “Patients with disease for a 6-month period or longer have a higher rate of DRIL,” said Dr. Singh. “With chronic edema,” added Dr. Shah, “the bipolar cells may get stretched beyond their limit, preventing transmission of signals from photoreceptors to ganglion cells and leading to poor visual outcomes.”
Dr. Wykoff noted that the more central the DRIL, the worse the outcome. “Involvement of the immediate parafoveal area is most relevant,” he said, “and disorganization in the midperipheral macula may have less impact on visual function.”
Changes over time. Because changes occur over time, studies typically use a marker of 3 to 4 months for determining when DRIL really sets in, said Dr. Shah, adding that DRIL may also resolve. Pharmacological treatments that improve retinal anatomy by reducing macular edema also appear to stabilize and, in some cases, improve the retinal vasculature,4 said Dr. Wykoff. “The relationships between DRIL, the retinal vasculature, and our treatments needs further study.”
3 Tips for Identifying Disorganization
With current technologies, identifying DRIL is a bit subjective, said Dr. Wykoff. “No OCT computer algorithm allows you to get a binary ‘yes’ or ‘no’ for the presence of DRIL.” But these steps may help add greater certainty:
- Have the photographer preset segmentation. An automatic algorithm allows fast and accurate segmentation of OCT volume data in the macular region, so that boundaries are aligned from scan to scan, said Dr. Shah. “One photograph gives us all the layers, facilitating comparisons.”
- Look at the OCT scan from the bottom up. This is important, said Dr. Shah, because retina experts have been predicting vision based on things that are too superficial. “You can have two patients with the same thickness, but two different types of pathology.” It’s important, he adds, to take a little extra time to evaluate morphology, and not just thickness.
- Examine the middle or periphery of the macula. Outside of the central macula, find the delineation between the inner retinal layers where the health of the retina looks preserved, said Dr. Wykoff. “Follow those intact interfaces toward the fovea,” he said. “If you can follow that segmentation border zone all the way to the fovea, then there is no DRIL. But if it breaks down and you can’t trace that border all the way to the fovea, DRIL is present.”
|
OCT May Connect the Dots
Even though imaging is readily available, noninvasive, and reproducible from machine to machine, said Dr. Wykoff, few clinical trials have used OCT findings as a primary endpoint. “Almost all phase 3 trials aimed at FDA approval of medications in the retina space have used visual acuity endpoints,” he said, “and that’s also what patients care most about: vision.” But OCT, and biomarkers like DRIL in particular, have the potential to help connect the dots between objective imaging and a vision endpoint.
Reproducibility. Correlating DRIL and visual outcomes may prove particularly helpful, said Dr. Wykoff, especially since methods for measuring VA have shortcomings: In many cases, standardized ETDRS testing used in clinical trials is not directly relevant to clinical practice, and Snellen visual acuity can be highly variable.
“But with eye-tracking software,” he said, “we have highly reproducible OCT scans and can track to the micron how well patients are doing.” Automated software allows us to look at DRIL and compare layers, scan by scan, said Dr. Shah. “This makes [detection of DRIL] easier, but [OCT] is sometimes not used to its maximum potential.”
Versatility. In addition, he said, OCT angiography allows visualization of both anatomy and physiology as well as a better view of the function of the deep capillary plexus (DCP), which provides about 15% to 20% of the oxygen to the photoreceptors. “If DRIL is a problem, there’s probably a DCP problem as well, which may have implications for future treatment.”
Moving toward consensus. Even with OCT’s advantages, however, DRIL is not quite ready for prime time, said Dr. Singh. “There’s a need for consensus guidelines as well as specific guidance for imaging techniques.” Dr. Wykoff agreed, “We still don’t fully understand what the threshold is for the disorganization to correlate with prognosis. How big an area must it be—50 microns, 100 microns, 400 microns? And what about disorganization of just 1 of the boundaries, not 2 or 3?”
Lack of consensus contributes to interobserver variability, said Dr. Singh. However, Dr. Sun and colleagues’ work has enhanced clarity and confidence by identifying the extent of DRIL associated with poor visual outcomes.
More at the Meeting
Use the AcademyPlus course pass to attend retina courses, such as:
Vitreoretinal Surgical Rounds: What Would Machemer Do? (202). When: Sunday, Nov. 12, 10:15 a.m.-12:30 p.m. Where: Room 398.
Advanced OCT Diagnosis (454). When: Monday, Nov 13, 11:30 a.m.-12:30 p.m. Where: Room 391.
The Cutting Edge of Pathologic Myopia (522). When: Monday, Nov. 13, 11:30 a.m.-12:30 p.m. Where: Room 282.
Advanced Vitreoretinal Surgical Techniques (674). When: Tuesday, Nov. 14, 10:15 a.m.-12:30 p.m. Where: Room 391.
OCT Angiography in Retinal Diseases (653). When: Tuesday, Nov. 14, 12:45-3:00 p.m. Where: Room 396.
|
Benefits of Identifying DRIL
Used mainly as a research tool today, DRIL will likely continue to add greater value in the clinic, said Dr. Singh.
Predict outcomes. Dr. Wykoff cites two clinical situations where identifying DRIL may be helpful with prognostication. He finds it most useful clinically for patients with macular edema in whom the retina has been dried with pharmaceuticals and the retina looks much better, but vision is not as good as expected or desired. “There is value at this point in considering the integrity and organization of the retinal layers,” said Dr. Wykoff. “If you see DRIL, it may be an indication that vision is impaired because of damage to the retina beyond just swelling.”
The other case would be for a patient with edema who has not yet been treated. “If there is extensive DRIL, that may help you set realistic expectations for the patient,” said Dr. Wykoff. “You can tell the patient that there are options to help with the edema, but that you have concerns about the ultimate prognosis due to disorganization of the inner retinal layers.” However, Dr. Wykoff is hesitant to overuse it in these cases since patients can have DRIL and still do well.
Manage expectations. DRIL may also aid in managing expectations by providing patients with a better understanding of their disease process and why their vision may not ever be what they desire, said Dr. Singh. He gives another example of a patient with DME preparing for cataract surgery. “After surgery, a patient who’s had DRIL for a while and not received treatment might only achieve minor visual improvement, not 20/20.”
Tailor therapy. DRIL might become an imaging biomarker that physicians can use to classify patients—to better understand when to treat and which therapies might work best, said Dr. Singh. For instance, more accurate prognostication may help patients avoid unnecessary DME treatment, he said, which is intensive, requiring 8 to 10 injections over a 1-year period.
Although theoretical at this point, it’s possible that certain drugs may work better for problems with the superficial plexus versus the deep capillary plexus—increasing the predictive value of DRIL, said Dr. Shah.
More Study Needed
Larger and longer studies are needed to gather more information about DRIL, said Dr. Singh. The hope is that it may one day lead to new practice guidelines similar to those developed for age-related macular degeneration, where an imaging biomarker called outer retina tubulation is seen in patients with higher rates of geographic atrophy.
In any event, DRIL is an important step forward, said Dr. Wykoff, providing a reminder of the need to be very specific and nuanced in the way we look at OCT images. “Hopefully, it is a part of a continuing evolution in analyzing imaging, understanding prognostication, and tailoring therapies for our patients.”
___________________________
1 Ou WC et al. Am J Ophthalmol. 2017;180:8-17.
2 Sun JK et al. JAMA Ophthalmol. 2014;132(11):1309-1316.
3 Sun JK et al. Diabetes. 2015;64(7):2560-2570.
4 Campochiaro PA et al. Ophthalmology. 2014;121(9):1783-1789.
___________________________
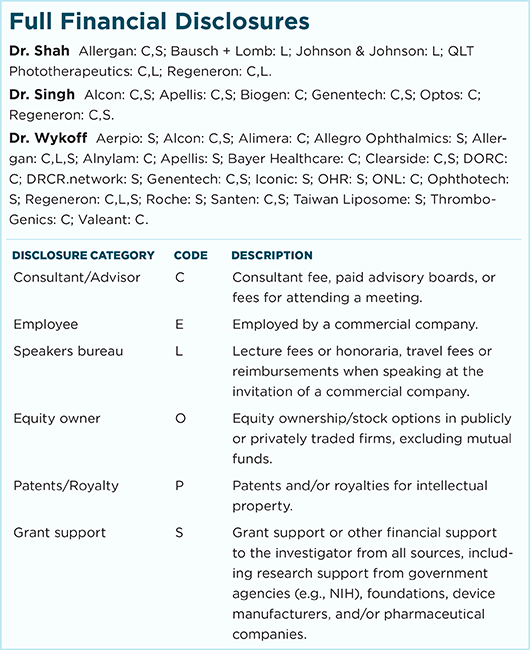
Dr. Shah is a specialist and codirector of retina fellowship at The Retina Institute in St. Louis, Mo. Relevant financial disclosures: None.
Dr. Singh is staff surgeon at the Cole Eye Institute, Cleveland Clinic, in Cleveland, Ohio. Relevant financial disclosures: Zeiss: C.
Dr. Wykoff is director of research at Retina Consultants of Houston. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.