Download PDF
Global interconnection, accelerating climate change, and viral evolution—the confluence of these and other factors may be magnifying the impact of certain viral infections that affect the eye.
“What we’ve seen with the spread of Zika and Ebola is that diseases thought to be limited in geographic scope are actually quite broad in their effect and, through travel, can potentially impact individuals on any continent,” said Allen O. Eghrari, MD, at the Wilmer Eye Institute in Baltimore.
 |
|
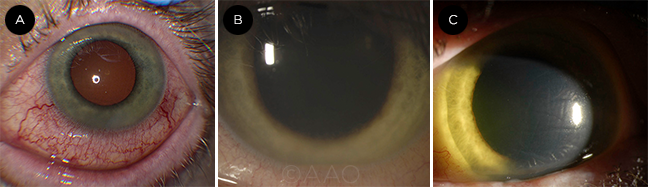
EBOLA. As panuveitis developed in this Ebola survivor, the slit-lamp photo showed diffuse anterior scleritis as inflammation worsened (A). This was followed by a layered hypopyon uveitis (B) and corneal edema with iris heterochromia (C).
|
A Look at Ebola
Ebola virus disease (EVD) is a viral hemorrhagic fever that can cause a range of severe symptoms, including high fevers, myalgias, severe diarrhea, and vomiting, said Steven Yeh, MD, at the Emory Eye Center in Atlanta. The outbreak of 2013-2016 was the largest and most fatal ever—leading to more than 11,000 deaths among more than 28,600 people affected.1
Ophthalmology in the trenches. Dr. Yeh was part of a team at Emory Eye Center that cared for the sight-threatening eye disease of Ian Crozier, MD, who contracted life-threatening EVD while treating patients in Sierra Leone. (At the time, the Emory team included Dr. Yeh’s colleagues Jessica G. Shantha, MD, and Brent Hayek, MD.)
Dr. Eghrari and Rachael J. Bishop, MD, MPH, from the National Eye Institute, each spent 4 to 5 months on the ground examining patients in Liberia during and after the Ebola outbreaks, and they now lead an eye program there.
A perfect storm. With EVD, “patients develop severe electrolyte abnormalities [due to volume loss] and subsequently can have cardiac arrest as well as septic or hypotensive shock from a severe inflammatory reaction and high viral load,” said Dr. Yeh. “Patients develop a cytokine storm, which can develop into an intravascular process leading to bleeding and mucosal or cerebral hemorrhages.”
Making the diagnosis. Polymerase chain reaction (PCR) testing of serum can confirm the diagnosis in the initial stages of the disease, said Dr. Yeh. Other tests, which require validation and further study, include virus-specific testing for immunoglobulin M (IgM) and immunoglobulin G (IgG) antibodies.
The Malevolent Mosquito
Ebola and ZIKV aren’t the only mosquito-borne viruses that pose a threat to the eye.
Epidemiologists are tracking the spread of chikungunya, dengue fever, yellow fever, and West Nile disease around the world. While dengue fever, yellow fever, and West Nile are closely related to ZIKV, chikungunya is not, although it is transmitted by the same mosquito that transmits ZIKV.
“Most of these diseases originated in East Africa,” said Lee M. Jampol, MD, at Northwestern University in Chicago. And with the possible exception of yellow fever, all are possible causes of inflammation in the eye, he said. There are no systemic treatments for these particular viral infections, Dr. Jampol said. All the clinician can do is provide supportive therapy.
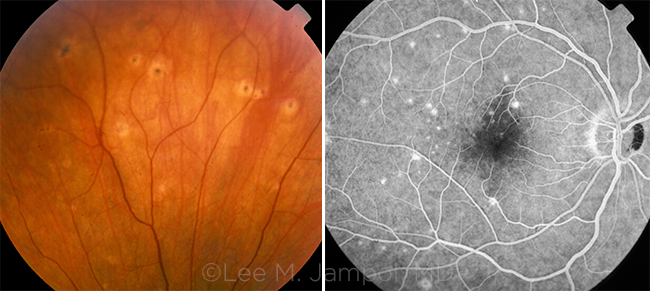
A note on West Nile. West Nile is now present throughout the continental United States, said Dr. Jampol. His research group was the first to describe its effects on the retina in adults as the disease spread across the United States in the late 1990s.
Characteristic ocular pattern. Most patients with West Nile are asymptomatic, and lesions in the retina tend to heal, Dr. Jampol said. The ophthalmologist may see tiny foci of inflammation. These foci may occur in a linear pattern; alternatively, they may be scattered, said Dr. Jampol. “Most uveitis and retinal specialists can diagnose West Nile based on its appearance.”
It’s critical to note that in diabetic patients, the virus can produce a much more severe effect on the retina and can cause retinal ischemia. People with diabetes may develop severe retinopathy and need treatment, either with laser or anti-VEGF treatments.
Threat to the brain. Spotting signs of West Nile in the eye helps with diagnosis in the brain, said Dr. Jampol. “No one has isolated it [the virus] from the eye, but we are quite certain it is there because an active process in the eye coincides with the presence of encephalitis.”
|
Ebola and the Eye
During the acute stage of the illness, which occurs anywhere from 2 to 21 days following exposure, common ocular signs and symptoms include pain, light sensitivity, blurred vision, floaters, inflammation, and conjunctival hemorrhage, said Dr. Yeh. “Some of our patients reported profound vision loss at the time they were hospitalized in Ebola treatment units.” However, during this acute phase, vision issues may be less urgent than the supportive care needed to save lives, he added.
Sicker patients, sicker eyes? With Ebola, uveitis is the most common finding, and it can be sight-threatening or even blinding, said Dr. Yeh. A high concentration of virus during the acute disease is associated with development of uveitis. Conjunctival injection during the acute phase of EVD has also been associated with uveitis.2
“The longer [that] survivors were in the Ebola treatment unit,” added Dr. Eghrari, “the more likely they were to develop uveitis and associated complications, suggesting that those who were sicker were more at risk for uveitis.”
However, a recent study out of Liberia found a weak correlation between patient-reported symptoms and ocular manifestations, said Dr. Yeh. “What that tells us is that all survivors should have an ophthalmic evaluation to identify the possibility of uveitis, not just those who are symptomatic.”
Sequelae. The Emory ophthalmologists found that 25% of Ebola survivors developed uveitis or optic nerve disease, and 40% had severe vision impairment or blindness, according to World Health Organization (WHO) criteria.
“In survivor after survivor, we’ve seen that virtually any part of the eye can be affected,” said Dr. Eghrari. For example, inflammatory changes in the eye can induce posterior synechiae, cataract, epiretinal membrane, macular chorioretinal scarring, or optic disc swelling—all of which can cause vision changes in Ebola survivors. Neurological deficits can also contribute to vision loss, he said.
Unique to Ebola. Patterns of macular edema—some focal, some diffuse—appear unique to Ebola survivors compared with controls, said Dr. Eghrari. “We also see multifocal retinal lesions that appear specific to Ebola virus disease and whose features change over time.”
 |
|
CHORIORETINAL SCARS FROM WEST NILE VIRUS, in fundus photo and autofluorescence. According to the CDC, 2,038 cases of West Nile disease were reported in 2016 in the United States. Of those, 56% were neuroinvasive in nature.
|
Caring for Survivors
Many survivors of EVD are quite young, said Dr. Eghrari. This makes it particularly important to holistically address a wide range of eye problems that can occur in the setting of the disease.
“Treating people with Ebola eye disease has to be comprehensive,” Dr. Eghrari said. For instance, some survivors experience changes that may cause an increase or decrease in intraocular pressure, while others may have conditions such as syphilis or herpetic eye disease that may be exacerbated in the presence of an acute illness.
Drug therapy. In West Africa, patients have responded to corticosteroids, said Dr. Yeh. “If an active infection is present, it may require an anti-infective agent as well as the steroids to treat the inflammation. We treated Dr. Crozier with a combination of topical and systemic corticosteroids and local corticosteroid injections in addition to an experimental antiviral drug.”
Some patients have irreversible vision loss, said Dr. Yeh. Others have developed mild or moderate impairment. “But some of the patients we treated with topical and systemic corticosteroids have recovered vision, which is really gratifying.”
Ongoing monitoring. The Partnership for Research on Ebola Virus in Liberia (PREVAIL) has recruited a group of 3,000 Liberian Ebola survivors and their close contacts who will be followed for 5 years until 2020. The Liberia-U.S. clinical research partnership will specifically evaluate long-term health consequences, development of immunity, and transmission of the disease. The study will also provide the largest-ever pool for studying Ebola eye disease, said Dr. Eghrari.3
Using serology. All participants in the PREVAIL study have been tested for the presence of antibodies, said Dr. Eghrari. This can confirm contact with the virus and makes it possible to specifically associate changes with the virus.
Serology also allows the physicians to rule out co-infection with other viral diseases and screen for other causes of eye problems. For instance, Dr. Eghrari said, “Ocular surface disease is very common in West Africa, and many symptoms such as ocular discomfort, sensitivity to light, irritation, redness, or even discharge have been found in a high proportion of our control participants.”
Tracking changes. During annual follow-up of patients in Liberia, the clinic staff use optical coherence tomography (OCT) to look for any subtle changes, said Dr. Eghrari. “This allows us to look for any changes and for responses to treatment, even when subjective measures of visual acuity might remain quite good. With OCT, we’ve been able to identify objective decreases in intraocular inflammation after treatment with steroids.”
Hiding in plain sight. As was the case with Dr. Crozier, high concentrations of the virus can persist in the eye, an immune-privileged system.4 (Ebola virus can also persist in semen for 12 months or more.5) “Although we know the virus can persist in the eye for some time, it’s unclear where the virus is sequestered, because a number of structures could serve as havens,” said Dr. Eghrari.
This viral persistence may increase the risk of Ebola exposure to care providers who perform surgeries such as cataract or vitreoretinal surgery, said Dr. Yeh. “To address this question, we initiated a study in Sierra Leone called Ebola Virus Persistence in Ocular Tissues and Fluids [EVICT] Study.”
 |
|
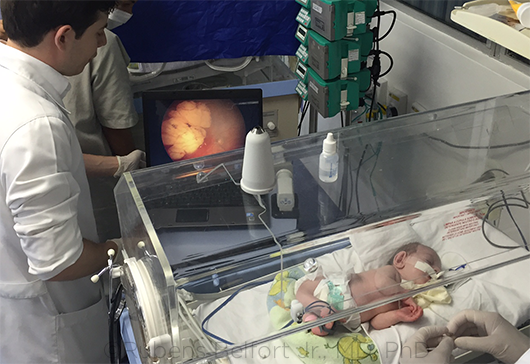
ONGOING DIFFICULTIES. Severe microcephaly, as seen in this infant, presents clinicians with a unique set of challenges.
|
A Look at Zika
Present in Africa for about 60 years, Zika virus (ZIKV) is among a group of RNA-based flaviviruses that are transmitted to humans mostly by the Aedes aegypti and A. albopictus mosquitoes. It has the ability to spread quickly, said Rubens Belfort Jr., MD, PhD, at the Federal University of São Paulo in Brazil.
Potent strain. Responsible for the most recent epidemic, an Asian strain of the virus likely made its way to northeastern Brazil from Micronesia, possibly by way of an athletic competition, Dr. Belfort said (see “Understanding Zika Strains”).
There are “no reports in the literature that ZIKV caused microcephaly in Africa,” said Camila Ventura, MD, at the Bascom Palmer Eye Institute in Miami. However, in Brazil, the damage in newborns has been devastating, causing neurological, skeletal, ocular, and hearing abnormalities, she said. This cluster of abnormalities is now known as congenital Zika syndrome (CZS).
Epicenter: Brazil. The virus started to infect people in Brazil about 2 years ago, said Dr. Belfort, and then in the fall of 2015, a large number of children were born with CZS.
“We were screening for retinopathy of prematurity when we started seeing babies with ocular lesions and smaller-than-normal heads,” said Dr. Ventura. “Given the new, more serious manifestations of the disease, it was first necessary to prove that Zika was causing it, and then show that the virus was capable of replicating in and crossing the placenta using trophoblasts as the reservoir.”
Milder elsewhere? Although cases of ZIKV have been reported throughout the world, the outcomes have thus far been less devastating than in Brazil. For instance, in the United States, the Zika Pregnancy Registry recently estimated that only 6% of infants exposed to Zika during pregnancy have developed birth defects, said Dr. Ventura. Some researchers have hypothesized that birth defects in Brazil may be worse due to prior exposure to dengue virus.6
Zika in adults. The acquired infection in adults looks very different from that in babies with CZS. During the first trimester, some mothers have reported systemic symptoms such as skin rash, arthralgia, and fever, said Dr. Ventura, but among 100 mothers examined by her team in Brazil, none reported ocular symptoms during pregnancy. “We have, however, seen reports of conjunctivitis, anterior uveitis, acute maculopathy, and posterior uveitis in adults,” she said. “As soon as the viremia is gone, however, patients recover their vision completely and experience no sequelae.”
Complete recovery also occurred in a 64-year-old U.S. resident who was diagnosed with ZIKV retinopathy following a mission trip to the Caribbean. The patient’s disease course and clinical appearance were consistent with unilateral acute idiopathic maculopathy; the diagnosis was pinned down via use of the serum plaque reduction neutralization technique (PRNT) assay.7
Zika in infants. Today, a multidisciplinary team in Recife, Brazil, is following about 300 babies who have a range of manifestations. In infants, some systemic findings are shared with other infections such as cytomegalovirus (CMV) and toxoplasmosis, said Dr. Ventura, including intracranial complications, microcephaly, seizures, developmental delays, and hearing loss. However, she said, the following combination of findings is unique to CZS: 1) severe microcephaly with partially collapsed skull; 2) brain abnormalities, including thin cerebral cortices, ventriculomegaly, and subcortical calcifications; 3) macular scarring and focal pigmentary retinal mottling; 4) congenital contractures, including arthrogryposis and clubfoot; and 5) marked early hypertonia and symptoms of extrapyramidal involvement.
Some children who were born without microcephaly later developed this finding, as well as other neurodevelopmental problems, said Dr. Belfort. “Therefore, [congenital] microcephaly is no longer needed to make a diagnosis.”
Making the diagnosis. PCR can help diagnose ZIKV during the first 2 weeks of acquired infection, but this is rarely done given that symptoms are often mild in adults, said Dr. Belfort. However, if a pregnant woman is diagnosed with the disease, clinical and ultrasound exams can be used to identify microcephaly and other neurological malformations in the fetus, he added.
Diagnostic challenges. After the acute phase, IgM testing for antibodies in blood, urine, cord blood, or cerebrospinal fluid can suggest exposure, but Zika has high cross-reactivity with other flaviviruses.8 Thus, presumed positive, equivocal, or inconclusive tests must be forwarded to the CDC or a CDC-designated lab for confirmation with PRNT testing.8
In addition to missed diagnoses in adults, there are economic barriers to diagnosis, said Dr. Belfort, because all the tests are very expensive. Finally, with Zika, it’s also important to rule out other conditions, he added, such as syphilis, toxoplasmosis, herpes, and HIV.
 |
|
EXAM FINDINGS. ZIKV can affect both the anterior and posterior parts of the eye. In this instance, a large ZIKV lesion is evident in the posterior pole of the infant’s eye.
|
Congenital Zika and the Eye
What to look for. Ocular findings are more common in infants who have severe microcephaly and were infected during the first trimester of pregnancy.9 Both the posterior and anterior parts of the eye may be affected, said Dr. Belfort. However, the most common ocular findings identified in these children are a well-demarcated chorioretinal scar in the macular region and focal pigment mottling, not an active uveitis, said Dr. Ventura.
“Although not common, retinal hemorrhages, abnormal retinal vessels, microphthalmia, iris changes, and cataracts may also be present,” Dr. Ventura said. In addition, Dr. Belfort and his colleagues published a case report of congenital glaucoma associated with Zika infection.10
Optic nerve involvement. Van den Pol et al.11 analyzed the eyes of infected mice to better understand the pathophysiology of microcephaly and ocular involvement in CZS, said Dr. Ventura. “The first cells infected were astrocytes in the brain and the glial cells in the optic nerve and retina. The same study showed that ZIKV spreads to other parts of the brain, including the central nervous visual system [retina, optic chiasm, suprachiasmatic nucleus, lateral geniculate nucleus, and/or superior colliculus] by axonal transportation.”
In another mouse study, Singh et al. found that several types of retinal cells are permissive to ZIKV replication and express receptors for entry.12
Vision loss and rehab. “Virtually all the babies we have seen present with severe visual loss,” said Dr. Ventura. “We have also observed that many develop strabismus and nystagmus with time. Surprisingly, [some] babies present with visual impairment even in the absence of ocular findings. Thus, vision loss appears more related to brain damage than to ocular damage itself.”
Since children have a high level of neuroplasticity, the main goal of visual rehabilitation, Dr. Ventura added, is to encourage new brain connections to better develop vision.
Long-term outcomes. “The clinical picture of Zika is probably more complex than we first knew,” said Dr. Belfort. “These kids are now 1 year old, and we do not know what will happen with them—whether their retinal lesions will reactivate or whether they will present with new lesions. It will be important to continue to follow them.”
Impact on corneal grafts. Now that ZIKV has been isolated in tears, and organ transplants have been reported as a mode of transmission of ZIKV, said Dr. Ventura, ophthalmologists have become concerned about corneal transplants. Research is now under way on the risk of contracting the virus from a corneal graft, she said.
|
Understanding Zika Strains
The African and Asian strains of ZIKV are genetically similar, said Dr. Ventura.
However, in a mouse model experiment, the Asian strain caused a higher upregulation of p53, a protein that regulates the cell cycle.1 “This finding suggests that p53 plays a pivotal role inducing apoptosis in human cortical neural progenitor cells, affecting the normal development of the central nervous system,” said Dr. Ventura. “It may help explain why brain injuries are more prevalent in babies with this strain of Zika.”
In other mouse model experiments,2,3 only the mice that lacked type I interferon (IFN) receptor presented with severe neurological disease after being exposed to ZIKV, a finding that is compatible with those seen in humans. During development, type I IFN response rises with age and is considered the first line of defense against viral infections in the brain. Thus, scientists currently think that type I IFN is key to understanding the pathophysiology behind congenital Zika syndrome, Dr. Ventura said.
___________________________
1 Zhang F et al. Nucleic Acids Res. 2016;44(18):8610-8620.
2 Lazear HM et al. Cell Host Microbe. 2016;19(5):720-730.
3 Rossi SL et al. Am J Trop Med Hyg. 2016;94(6):1362-1369.
|
What the Future Holds
The newer outbreaks of both Zika and Ebola appear to be greater both in severity and in magnitude than previous outbreaks, said Dr. Eghrari. That realization is generating support for a number of strategies, including the following.
Monitoring systems. Building systems to sup- port lab and genetic evaluation of viruses may prove extremely valuable for identifying genetic markers that can be followed during and after an epidemic, Dr. Eghrari said. “Subtle changes that occur over the course of transmission from person to person make it possible to link cases to previous outbreaks.”
Collaboration. “We’ve seen collaboration among individuals and institutions working together to research Ebola and Zika eye disease,” said Dr. Eghrari. “This has helped in building capacity and pooling information, human resources, and medications, in addition to developing vaccines.” The hope is that lessons from recent outbreaks will contribute to the understanding of future problems, he said, making it possible to address issues as they arise and prevent outbreaks from causing pathology on a larger scale.
Hector the vector. Without prevention, the WHO estimates that around 4 million people could be affected by ZIKV by 2020. Prevention is the only way to control diseases like this, said Dr. Belfort. “We’ve been fighting mosquitos for more than 100 years, but the mosquitos are winning. Malaria continues to be out of control. Yellow fever is back in Africa, and, we had a new outbreak of yellow fever in Brazil. Unless we win against mosquitos and improve social and economic conditions, we’ll have an outbreak a month.”
Vaccines. In addition to mosquito abatement, the other critical preventive approach is vaccination. A vaccine trial for ZIKV is under way.13
And, led by the WHO and partners, an Ebola vaccine trial in Guinea and Sierra Leone showed significant efficacy with a vaccine using a ring vaccination algorithm, said Dr. Yeh. “People who had close contact and contacts of those who had close contact with Ebola [i.e., drawing a ring around the index case] were vaccinated. Ten days after the vaccination, there were no cases of Ebola.”
The role of ophthalmology. It’s important to remind clinicians that they can play an important role in diagnosis, Dr. Ventura said. “With Zika, many people were speculating at first that a batch of expired rubella vaccine was responsible for the brain injuries in newborns. After publishing the first article describing the ocular findings14—which were completely different from those caused by congenital rubella—we could say, ‘We don’t know what this is yet, but it is not rubella.’”
___________________________
1 World Health Organization. Ebola Outbreak 2014-2015. Accessed Feb. 27, 2017.
2 Mattia JG et al. Lancet Infect Dis. 2016;16(3):331-338.
3 National Institutes of Health. Study of Ebola Survivors Opens in Liberia. Accessed Feb. 27, 2017.
4 Varkey JB et al. N Engl J Med. 2015;372(5):2423-2427.
5 Centers for Disease Control and Prevention. Traces of Ebola Virus Linger Longer Than Expected in Semen. Accessed Feb. 27, 2017.
6 Muller WJ, Miller ES. JAMA. 2017;317(1):35-36.
7 Parke DW III et al. Ophthalmology. 2016;123(11):2432-2433.
8 Centers for Disease Control and Prevention. Diagnostic Tests for Zika Virus. Accessed April 10, 2017.
9 Ventura CV et al. JAMA Ophthalmol. 2016;134(8):912-918.
10 de Paula Freitas B et al. Ophthalmology. 2017;124(3):407-408.
11 Van den Pol AN et al. J Neurosci. 2017;37(8):2161-2175.
12 Singh PK et al. JCI Insight. 2017;2(4):e92340. doi:10.1172/jci.insight.92340.
13 Abbasi J. JAMA. 2016;316(12):1249.
14 Ventura CV et al. Lancet. 2016;387(10015):228.
 |
|
These images are from PREVAIL, the Liberia-U.S. clinical research partnership, which is expected to provide the largest-ever pool for studying Ebola eye disease.
|
For Further Reading
Caviness K et al. Ebola virus persistence as a new focus in clinical research. Curr Opin Virol. 2017;23:43-48. doi:10.1016/j.coviro.2017.02.006. [Epub ahead of print.]
Cragan JD et al. Baseline prevalence of birth defects associated with congenital Zika virus infection–Massachusetts, North Carolina, and Atlanta, Ga., 2013-2014. MMWR Morb Mortal Wkly Rep. 2017;66(8):219-222.
Ikejezie J et al. Zika virus transmission–region of the Americas, May 15, 2015-Dec. 15, 2016. MMWR Morb Mortal Wkly Rep. 2017;66(12):329-334.
Peak CM et al. Comparing nonpharmaceutical interventions for containing emerging epidemics. Proc Natl Acad Sci USA. 2017;pii:201616438. doi:10.1073/pnas.1616438114. [Epub ahead of print.]
|
Meet the Experts
Rubens Belfort Jr., MD, PhD Professor and chairman of ophthalmology at the Federal University of São Paulo in São Paulo, Brazil. Relevant financial disclosures: None.
Allen O. Eghrari, MD Assistant professor of ophthalmology at the Wilmer Eye Institute in Baltimore. Relevant financial disclosures: None.
Lee M. Jampol, MD Professor of ophthalmology at Northwestern University in Chicago. Relevant financial disclosures: None.
Camila Ventura, MD Pediatric retina research fellow at the Bascom Palmer Eye Institute in Miami and retina specialist at the Altino Ventura Foundation in Recife, Brazil. Relevant financial disclosures: None.
Steven Yeh, MD Louis M. Simpson Professor of Ophthalmology and director of the Uveitis and Vasculitis Section at the Emory Eye Center in Atlanta. Relevant financial disclosures: Santen: C.
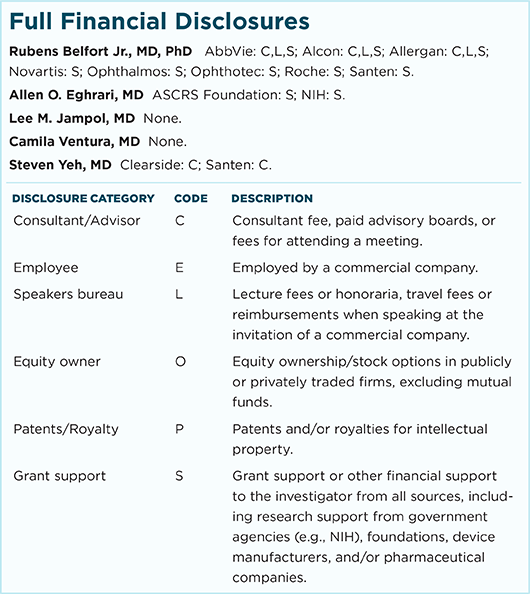
For full disclosures and the disclosure key, see below.
|