This article is from October 2004 and may contain outdated material.
When the Ex-Press shunt was first introduced for open-angle glaucoma, it was marketed as an innovative treatment for the reduction of IOP when other more conventional treatments have failed. Moreover, it was touted as a device that could be quickly implanted with a minimally invasive approach.
As with many new devices, however, the Ex-Press stumbled. “The first procedure, [in which the device was placed] under a conjunctival flap, was a good idea,” said Marlene R. Moster, MD, clinical professor of ophthalmology at Thomas Jefferson University and attending surgeon at Wills Eye Hospital in Philadelphia. “It was quick. It was simple. The delivery system was easy to do.” But, she added, the postoperative complications—profound hypotony, shallow chambers and slow visual recovery—were unacceptable.
However, Dr. Moster, who has used the Ex-Press in intractable eyes with a history of previous glaucoma surgery, is cautiously optimistic that the shunt may find a surgical home, thanks to modifications to the original surgical procedure. In particular, she said, it may prove to be effective in cases where the physician may not want to repeat a trabeculectomy after the first has failed, yet may want to reserve the larger tube shunt for the future.
 |
|
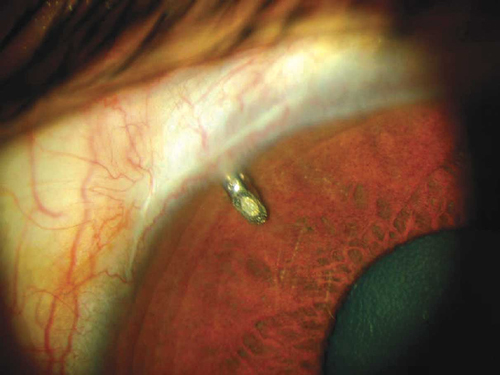
When used under a scleral flap, as shown here, the Ex-Press may serve as a go-between after a failed trabeculotomy and before shunt surgery. Photo credit: Optonol Ltd.
|
Original Specs
What it is. The Ex-Press was developed by Optonol Ltd., a private Swiss-Israeli company. It was designed to reduce IOP by diverting excess aqueous humor from the anterior chamber to a subconjunctival bleb. The tube, which is made from implantable stainless steel, is 2.5 millimeters long and 400 micrometers in diameter. The Ex-Press was intended for use with or without mitomycin C, and either alone or in conjunction with cataract surgery.
Pros. Surgical time is short—reportedly, the device can be implanted in less than five minutes. Additionally, it can be inserted through a small incision in the conjunctiva.
Cons. Robert D. Fechtner, MD, who used the Ex-Press as intended in a few patients who were poor candidates for trabeculectomy or a drainage device, observed complications similar to those cited by Dr. Moster. “[The Ex-Press] was introduced with the enthusiastic hope that we would now have a fast, safe and effective glaucoma procedure. It turned out to be a fast and perhaps overly effective procedure, in that there were shallow chambers and low pressures in the early postop period,” said Dr. Fechtner, associate professor of ophthalmology at the University of Medicine and Dentistry of New Jersey, Newark.
Back to the Drawing Board
Given such complications, Dr. Moster might have abandoned the device. But then she heard about a group in South Africa that had modified the surgical technique. Instead of placing the Ex-Press under the conjunctiva, as its developers intended, they placed it under a scleral flap, where it behaves quite differently, she explained.
New approach. The revised surgical technique involves the creation of a fornix-based conjunctival flap and a 4- x 4-mm scleral flap. Dr. Moster then places two releasable sutures and uses mitomycin C. The aqueous flow starts immediately and percolates from the edges of the scleral flap posteriorly to form a low and diffuse bleb, she said.
Pros. With this new approach, the complication rate is markedly decreased, Dr. Moster said. She has observed only rare instances of shallow or flat chambers, few instances of choroidal effusion and fairly rapid return of visual acuity. There can be early hypotony within the first few days to a week, but by three weeks visual acuity in most patients has returned to preoperative levels. In most patients, IOP has fallen into the low or mid teens, and it has tended to remain at less than 20 mmHg, with little, if any, medication. There have been some complications, such as self-limited choroidal effusion, but these have been fewer than with the original technique, Dr. Moster said. There also have been fewer complications than might arise with either the Baerveldt or Ahmed tube shunts, which can have a 40 percent morbidity rate, she added.
The results using the Ex-Press under a scleral flap may be a bit more consistent than those of a repeat trabeculectomy. One possible explanation, said Dr. Moster, is that trabeculectomies are often tied up tightly for better control to avoid a flat anterior chamber. However, this may result in a high postop pressure and not enough flow under the flap, which is needed to establish a nice bleb. The Ex-Press under the scleral flap also avoids the situation in which too much aqueous escapes, resulting in precipitously low pressure. With the modified technique, the relationship between the scleral flap edge and the Ex-Press opening is the same each time, and the aqueous flow is constant. “Maybe this is why a nice bleb is established immediately and why it works,” Dr. Moster said. “You’re putting this little device right in the middle of a 4 x 4 flap. It’s consistent.”
Dr. Fechtner agreed that there may be a more predictable early outflow with the Ex-Press than with trabeculectomy. It’s possible, he said, that having a standardized 50-µm hole, which this device provides, would make early postop management easier. “On the other hand, there may be unexpected outcomes from the Ex-Press.”
Cons. When inserted under the scleral flap, the Ex-Press is no longer a minimally invasive, quickly inserted device. “It’s quick, but it’s not five minutes,” said Dr. Moster. “It’s a little bit shorter than a standard trabeculectomy.”
Cautions to consider. Dr. Moster cautioned that no one knows exactly how the device functions under the flap. She hypothesizes that there is a constant flow of aqueous through the Ex-Press opening that forms a scleral lake under the flap. Combined with two mildly tight sutures at the posterior end, and two releasable sutures closer to the limbus that can be removed at any time, there is much more control over this procedure than originally proposed with implantation under just the conjunctiva. “Posterior flow of aqueous through the scleral flap forms a low, diffuse bleb, which is satisfactory,” she said.
Dr. Fechtner added that no one knows what will happen over the long term with a surgical steel drain in the eye. “This material is used elsewhere in the body, but I don’t know of any other intraocular metal implants. I hope surgeons will continue to monitor these patients over the long term.”
Who Will Benefit?
When used under the scleral flap, the Ex-Press may find its niche in eyes that have had prior surgery but where a quadrant of mobile conjunctiva still remains, and where the IOP needs to be in the low teens. While such eyes typically would do best with either an excellent trabeculectomy or a shunt procedure, the Ex-Press may prove to be another alternative, given the high morbidity rates of shunts, Dr. Moster said. In its favor, she noted that the Ex-Press can be removed, if necessary. “If it fails, you can go to a tube.”
Further study is needed, Dr. Moster cautioned. In the meantime, she said, “The Ex-Press under a scleral flap may be a go-between after one trabeculectomy has failed and before you put in a shunt.”
Searching for a Niche
The fact that the Ex-Press surgical technique has changed is not unusual, said Dr. Fechtner. “New devices often go through a growth or experience phase.” He noted that, initially, some surgeons used a two-stage procedure with the Molteno implant to avoid shallow chambers and prolonged hypotony. In time, tube occlusion techniques were developed to minimize those complications so the procedure could be done in one stage. “I think that’s where the Ex-Press is,” he said.
It’s not known whether the Ex-Press will improve the outcomes achieved by standard trabeculectomy, Dr. Fechtner added. “Now we have to see whether the Ex-Press offers an advantage over the standard ways we are creating our ostiums.”
Both Drs. Fechtner and Moster agree that the device deserves more study. “At this time, we have noted fewer complications,” Dr. Moster said. “But we need a much longer follow-up.” Dr. Fechtner added, “I would not suggest we abandon the Ex-Press implant until I am sure that we have given thoughtful consideration to the ways it might enhance our surgery. Glaucoma surgery is ripe for innovation. The Ex-Press is a device searching for its best technique of implantation.”
_____________________________
Drs. Fechtner and Moster have no related financial interests.