By Leslie Burling-Phillips, Contributing Writer, interviewing Denise C. Fridl, COT, COE, CPPM, OCS, Aneesh Suneja, MBA, Robert E. Wiggins Jr., MD, MHA, and Joy Woodke, COE, OCS
Download PDF
Applying lean principles to your practice results in lower staff turnover, more revenue, and less overtime, and improves teamwork among staff—just to name a few of the tangible benefits,” said Aneesh Suneja, MBA, the coauthor of Lean Doctors and founder of FlowOne Consulting.
“The lean health care approach identifies what is of value to the patient and eliminates waste from each of the steps expended to provide that value,” said Robert E. Wiggins Jr., MD, MHA, a pediatric and neuro-ophthalmologist at Asheville Eye Associates in Asheville, N.C. Last month, EyeNet provided an overview of the lean approach; this month, the experts discuss how to get started and describe 2 key tools: the “waste walk” and the 5S method for evaluating and improving work processes.
Getting Started
Choose lean champions. While lean principles can improve processes for an entire organization, the initial change begins with 1 or 2 people. “Some practices employ 80 to 100 staff members, which makes it impractical to teach or reach a consensus on waste,” said Mr. Suneja. “The best approach is to select 1 or 2 physicians to advocate that going lean is critical for practice improvement.”
Start small. To avoid the common issues associated with change, you should begin on a small scale and then slowly move to a larger scale, so you can tweak and perfect each process before expanding into a wider scheme, said Denise Fridl, COT, COE, CPPM, OCS. Suppose, for example, you are thinking of moving the scheduling of follow-up appointments from the check-out to the exam room. “If you have 9 locations and 20 physicians, consider testing the change with 1 doctor. Only when you achieve success should you implement a change throughout the practice.” Ms. Fridl is chief performance officer at Asheville Eye Associates.
Experiment with changes in a controlled manner. As with any experiment, do not change too many variables simultaneously because it will be difficult to assess the impact of any one, said Mr. Suneja.
Early success can help foster a lean mindset. “As each improvement becomes salient, the value will be recognized by staff and physicians, which makes it easy to support the reasons for the change. The effect is palpable and comes in stark contrast to the top-down approach of mandating change that often provokes skepticism and resentment,” said Mr. Suneja.
When to Reassess Workflow
While it is important to periodically review your practice processes for inefficiencies (see “Look for 8 Types of Waste,” below), you also should reevaluate processes and make adjustments any time a significant change occurs. For example, when Oregon Eye Consultants implemented electronic health records, they conducted a comprehensive workflow analysis, said the practice’s administrator, Ms. Woodke.
“Practices are in a continually evolving environment, particularly due to federal health care rules and regulations,” said Mr. Suneja. Changes are frequent, and “every physician must decide how to incorporate a change into their practice, what impact it will have on the processes and the staff, and how it fits in the overall scheme of the practice or the organization.”
|
Look for Waste
“Waste is prolific in ophthalmology clinics, and identifying it is a critical element of any change management technique,” said Mr. Suneja. Fortunately, even small modifications can result in substantial improvements in patient, physician, and staff satisfaction—as well as benefits to your bottom line.
Perform a “waste walk.” In a waste walk, you can shadow patients, staff members, and physicians to identify waste, which is defined as use of resources that doesn’t add value. Identifying waste “is an important foundational step in the [lean] process. It does not take long for the proverbial ‘lightbulbs’ to illuminate your problem areas. This, in turn, causes a catalytic effect among the staff to seek additional sources of waste and motivates them to look for ways to improve their processes,” said Mr. Suneja.
“We assessed a patient encounter by following the entire exam process—from testing to optical to scheduling and surgery,” said Ms. Fridl. “This enabled us to identify areas of waste, improve our processes, and become more efficient,” she said.
Joy Woodke, COE, OCS, described how the waste walk was conducted at her practice, Oregon Eye Consultants. “We interviewed those who were performing certain daily tasks and asked them to walk through each process while we looked for instances where we were duplicating tasks or were not performing efficiently—and we eliminated as many steps within these procedures as possible. Then we tested the changes and asked for feedback before making permanent process modifications. Equally important, however, is regularly reexamining these workflows to determine if there is a new or better way to perform a process and eliminate steps or waste.”
Look for 8 types of waste. Last month’s Practice Perfect outlined the DOWNTIME mnemonic, which prompts you to watch for 8 types of waste: Defects, overproduction, waiting, nonused employee talent, transportation, inventory, motion, and excess (over-) processing. Once you have identified waste, it can, in many instances, be relatively easy to eliminate. For example, motion waste—defined as movement that does not add value—can be reduced by shifting supplies to a more efficient location, keeping additional supplies on hand, and placing regularly used items in an exam room.
Think Lean
In a September webinar, Mr. Suneja explained how to put lean principles into practice. Topics covered include:
- Eliminating waste through lean improvement techniques
- Evaluating and improving patient flow in your practice
- Prioritizing and problem-solving effectively
- Getting buy-in from others on process changes
- Maximizing use of equipment, such as the OCT, to reduce patient wait times
- Improving your scheduling process.
Access the webinar. If you missed the webinar, you can order a recording of Think Lean: Reduce Costs, Increase Profitability, and Improve Patient Satisfaction (product number: 0125069U) at aao.org/store.
For upcoming webinars, see aao.org/practice-management/webinars.
|
The 5S Tool for Reworking Processes
Sort, stabilize, shine, standardize, and sustain (or 5S) is Toyota’s system for evaluating and improving workplace organization. Applying this lean principle alone can have an enormous impact on reducing time expended on routine tasks and boosting your revenue. Here’s how it works.
1. Sort. Over time, a lot of items can accumulate in the office. Survey the accumulation, determine which items you need, and remove those that you don’t.
2. Stabilize (sometimes termed “set in order”). After removing the clutter, organize the remaining items to make them easily accessible to those who need them. Mr. Suneja said, “Simply reorganizing your front desk area and placing all the necessities within reach of your check-in staff can result in a huge cost savings. For example, if your clinic sees an average of 100 patients per day and you save just 1 minute of a worker’s time to check in each patient—that adds up to 100 minutes saved per day. When you multiply that over the course of the year, the net savings is approximately $9,000 in labor costs. It is amazing how these numbers can quickly add up.”
3. Shine. This doesn’t just mean keeping things clean—you also need to make sure that your practice’s tools, equipment, and other inventory are ready for use at any time.
4. Standardize. After you have followed the first 3 steps of 5S to create a leaner office, this fourth step ensures that you maintain the new efficiencies moving forward. This step can involve implementing new procedures and updating formal job responsibilities. You might also start performing regular checks to make sure that work areas are meeting the new standards of cleanliness, organization, and readiness. And you should periodically reassess workflow to see if new problems have emerged or old ones have resurfaced.
5. Sustain. Nurture a culture among physicians and staff that will help your practice to sustain a 5S approach over the long term.
The Long-Term Impact of Going Lean
How often does a physician have to wait for a patient to arrive in the exam room? If he or she loses 15 minutes per clinic, that adds up quickly. Assuming 4 clinic sessions per week, that would mean 1 hour lost every week. If this time had been spent attending to patients rather than waiting for them, the same physician could have seen an extra 300 patients during the course of a year. Estimate an office visit at $200 per patient, and you are losing about $60,000 per year. The bottom line: Focusing on the small things that impede schedules can produce meaningful results.
___________________________
Next month: Reduce patient wait times.
___________________________
Ms. Fridl is chief performance officer at Asheville Eye Associates in Asheville, N.C. Relevant financial disclosures: None.
Mr. Suneja is president of FlowOne Lean Consulting, based in Milwaukee, Wisc. Relevant financial disclosures: FlowOne Lean Consulting: C.
Dr. Wiggins is Academy senior secretary for ophthalmic practice and is managing partner at Asheville Eye Associates in Asheville, N.C. Relevant financial disclosures: None.
Ms. Woodke is administrator at Oregon Eye Consultants in Eugene. Relevant financial disclosures: None.
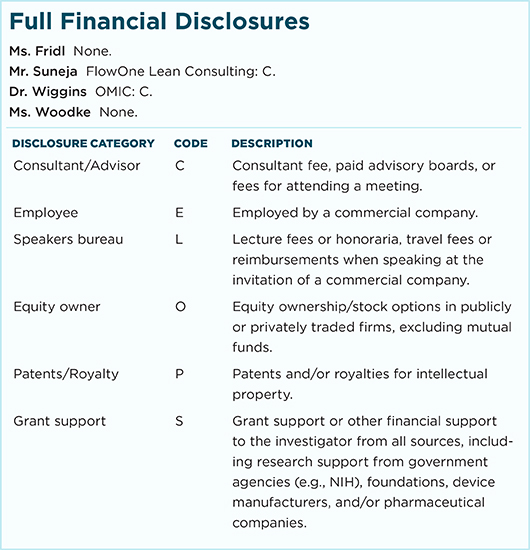
For full disclosures and the disclosure key, see below.