By Linda Roach, Contributing Writer, interviewing George H.H. Beiko, BM, BCH, FRCSC, Nicole R. Fram, MD, and Sadeer B. Hannush, MD
Download PDF
When lack of capsular and zonular support prevents placement of an intraocular lens (IOL) in the posterior chamber, some surgeons turn to sutureless intrascleral fixation of a 3-piece, posterior chamber IOL (PCIOL) as the solution.
Small Incision
Many ophthalmic surgeons who perform sutureless intrascleral fixation (also known as extracapsular fixation) say that this method of stabilizing IOLs, which uses a small-incision approach, represents an improvement over large-incision scleral suturing.
Indications. Intrascleral fixation is indicated in patients who have undergone traumatic injury or who have posterior capsular rupture, pseudoexfoliation, or other factors that have damaged the posterior capsule or weakened the zonules. These patients may have subluxations, crystalline lens fragments (or a dislocated IOL) in the vitreous, or visual problems from decentration, and they sometimes need a secondary implant.
Improvement. Before the development of intrascleral fixation methods, surgeons typically stabilized IOLs in problem eyes by suturing them to the sclera or the iris with polypropylene1 or, more recently, Gore-Tex (an off-label use), said George H.H. Beiko, BM, BCH, FRCSC, who practices in St. Catharines, Ontario, Canada. But iris-and scleral-sutured IOLs are not ideal, because of associated complications such as cystoid macular edema, postoperative inflammation, induced astigmatism, and late suture breakage, Dr. Beiko said.
 |
|
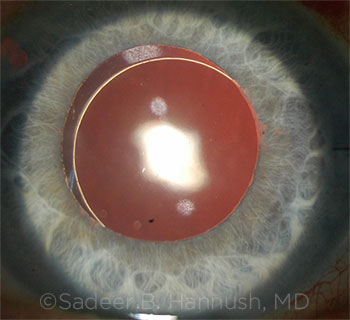
DAY 1 POSTOP. Sclerally fixated PCIOL using double-needle flanged haptic (Yamane) technique (dilated).
|
Two Techniques
Surgeons considering intrascleral fixation have 2 methods to consider.
Glue. Building on earlier work by Gabor B. Sharioth, MD, PhD, Amar Agarwal, MD, first published the glued IOL technique in 2008.2 For this technique, the surgeon uses forceps to place the lens haptics inside scleral tunnels, which are located underneath scleral flaps. The flaps are then repositioned over the haptics, and fibrin glue is applied to keep the flaps secure during the eye’s early healing.
Yamane. This newer intrascleral fixation method was developed by Shin Yamane, MD, and colleagues,3,4 and it is also known as the double-needle flanged haptic technique.
Using a pair of bent thin-walled, wide-bore 30-gauge needles, and with the IOL already in situ, the surgeon inserts the needles through the sclera 2 mm posterior to the limbus and feeds the PCIOL haptics into the lumen of the needles. The needles and sheathed haptics are then drawn out of the scleral tunnels, which simultaneously fixates the 2 haptics in those tunnels. The surgeon cauterizes the protruding end of each haptic, fashioning flanges that prevent the haptics from slipping back into the eye through the tunnels and dislocating internally.
 |
|
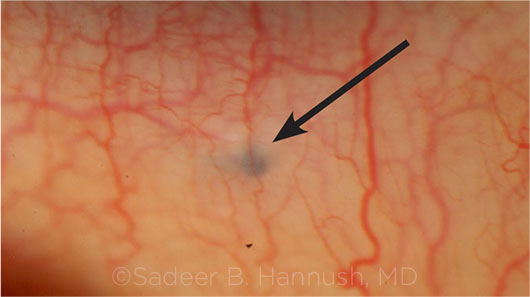
POSTOP. Flanged haptic end seen in the inferior subconjunctival space 2 mm from the limbus. (Arrow = haptic end.)
|
Choosing One Over the Other
Both methods are “wonderful techniques, because you can stay [with the] small incision, and this can potentially lead to faster visual recovery and possibly better refractive outcomes,” said Nicole R. Fram, MD, who practices in Los Angeles. That said, surgeons differ as to which technique they prefer to use (see also “Pros and Cons”).
Preference for glue. “I prefer the glued fixation method,” Dr. Beiko said. “I’ve been doing it for 7 or 8 years, and I use it about a dozen times a year. Dr. Agarwal’s technique is generally thought to be the first-line method for intrascleral fixation.”
Dr. Beiko said that after trying the Yamane technique in a few eyes and listening to presentations about it at international meetings, he concluded that the technique has problems that make it unsuitable for him to use.
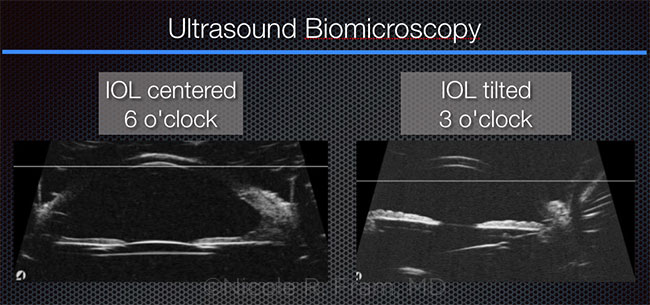
“What they found in Japan, in a prospective study, was more IOL tilt with the Yamane than with the glued technique,” Dr. Beiko said. Specifically, the study found that IOLs fixated with the Yamane method were tilted, on average, 13.2 degrees, compared to 4.8 degrees with the glued IOLs.5
“The other thing I’ve never been quite happy with is just blindly leaving the first haptic that’s been placed within the needle floating in the back of the eye while I’m fixating on the other haptic,” Dr. Beiko said. “I’m worried that this loose haptic, which is hidden behind the iris, might be touching the retina. It’s a perfect place to create a break in the retina if you touch it.”
Using both. Sadeer B. Hannush, MD, at Wills Eye Hospital in Philadelphia, said he began using the glue-assisted fixation technique 5 years ago, after Dr. Agarwal’s group reported that their IOLs had remained stable for several years after implantation. “In 2013, it became my preferred fixation method in eyes with inadequate capsular support, and it remains the gold standard in sutureless intrascleral haptic fixation,” Dr. Hannush said.
Dr. Hannush started exploring the Yamane technique in late 2016, after stumbling on an early paper describing the procedure. Today, he uses both approaches. He cautioned that the eye should remain pressurized at all times either with a chamber maintainer or with perfusion through a sclerotomy.
“I believe both techniques are here to stay, each offering advantages in certain settings and in the hands of the particular surgeon,” he said. “The glued IOL technique is very effective, and it may be a little bit easier to perform for surgeons who don’t do a lot of intrascleral fixation.”
Cautious about both. Dr. Fram said she has primarily been using scleral suture fixation and some glued IOL techniques over the past 10 years. In the last year, she said she has been evaluating the Yamane technique, because she views it as a clever small-incision technique with much promise. Another intriguing characteristic of the Yamane technique is that there is less hypotony associated with it in the early postoperative period, in comparison to larger-incision scleral suture fixation or even the glued IOL, she said.
But Dr. Fram is quick to point out that both intrascleral fixation methods are 2-point fixation and require symmetrical scleral tunneling and sclerotomy entries. Better standardization of these steps may improve outcomes, she said. “My experience with both the glued IOL and the Yamane technique is that critical steps of tunneling in the sclera and sclerotomy entry can be challenging in terms of reproducibility and standardization. Because this is 2-point fixation, IOL tilt is an issue.”
Out of the approximately 42 Yamane procedures Dr. Fram has performed, 4 IOLs had significant tilt, and 2 of them required refixation. “Interestingly, I had a patient who was 20/20 uncorrected—and as he healed over a 2-week period he developed 2.5 D of astigmatism,” she said. While corneal topography and wavefront analysis (OPD-Scan; Marco) revealed little corneal astigmatism, internal astigmatism > 2 D was detected. Ultrasound biomicroscopy confirmed the IOL was tilted, she said.
“So although there can be very rapid visual recovery, which makes for a wonderful procedure that you want to try, you have to be prepared and know how to refixate the IOL in the event that you get significant tilt,” she said. In addition, it is imperative that the surgeon examine the patient every 6 months for potential extrusion of the haptics subconjunctivally through potentially thin-walled scleral tunnels.
Pros and Cons
Dr. Hannush provided a concise overview of the 2 methods.
Glue: advantages.
- It compartmentalizes the eye nicely into anterior and posterior segments.
- It allows the use of foldable IOLs and thus a small corneal incision.
- All maneuvers are performed under direct visualization.
- The desired length of the haptic may be embedded in a scleral tunnel. This may be adjusted to optimize IOL centration and minimize rotation.
- It has a decade-long track record.
Glue: limitations.
- It requires familiarity with transscleral work, transferring the haptic from 1 forceps to the next (termed the “handshake technique” by Dr. Agarwal), as well as help from a third hand at certain points in surgery.
- It requires takedown of the conjunctiva and the creation of scleral flaps.
- It requires familiarity with the use of fibrin sealant.
- It requires familiarity with anterior vitrectomy techniques, ideally through the pars plana.
Yamane: advantages.
- The technique is conceptually simple.
- The need for conjunctival takedown and scleral flaps is obviated.
- It allows implantation of a foldable IOL through a small incision.
- It is currently the fastest method of sutureless PCIOL intrascleral haptic fixation.
- Eyes tend to be very quiet postoperatively with rapid visual rehabilitation.
Yamane: limitations.
- Despite its conceptual simplicity, it is surgically challenging even for a surgeon who is experienced in methods of scleral fixation.
- It requires familiarity with anterior vitrectomy techniques, ideally through the pars plana.
- As with the glued technique, and possibly more importantly, haptic placement is critical (180 degrees apart and 2 mm posterior to the limbus).
- The surgeon’s view is obstructed during the intrascleral passes.
- To decrease the chance of optic rotation, it is important to achieve at least a 2-mm tunnel during the intrascleral pass that is circumlinear with the limbus.
- Limited international experience.
|
 |
|
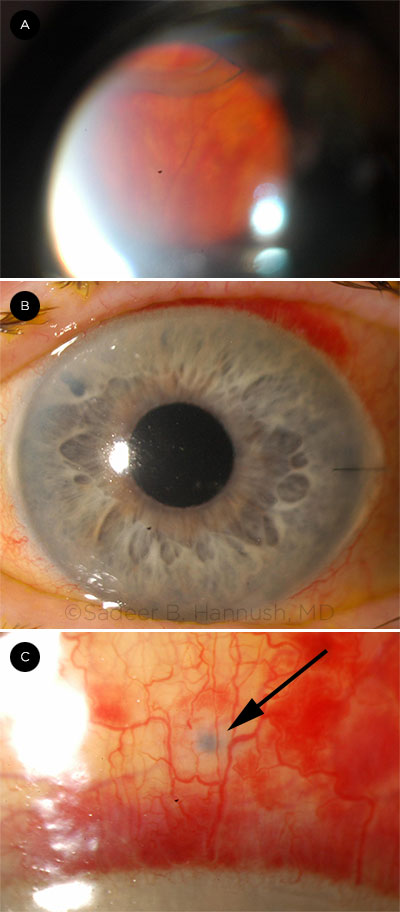
ANOTHER LOOK. Preop view of a posteriorly subluxated IOL (A). Postop view of the Yamane technique (undilated). Note the peripheral iridotomy superonasally (B). Postop view of the flanged haptic end in the superior subconjunctival space (C; arrow = blue haptic end).
|
Surgical Tips and Pearls
Two essentials. In order to do these procedures, “a surgeon should feel comfortable with a thorough triamcinolone-assisted anterior vitrectomy prior to the fixation portion of the procedure,” Dr. Fram said. “This is a must-have [technique] in your skill set, or else you shouldn’t be attaching anything to the wall of the eye.”
It also is essential to use an anterior chamber maintainer during these procedures, Dr. Beiko noted.
IOL selection. Dr. Beiko implants a 3-piece silicone IOL (LI61SE, Bausch + Lomb) for his glued intrascleral fixation cases. “But I think that virtually any 3-piece IOL can be used,” he said, with 1 exception: IOLs with PMMA haptics, because these are very friable.
Dr. Hannush said that specific IOL selection is crucial in Yamane cases, because conventional PMMA haptics are prone to kinking, breaking, or even disinserting from the optic during the potentially significant manipulation that the method involves. He recommends the EC-3 PAL lens (originally available from Aaren Scientific, now renamed Lucia 602 and available from Carl Zeiss), because its haptics are made from polyvinylidene fluoride, which is very resilient.
Special equipment. With the glued technique, conventional intraocular forceps should not be used, because they might damage the haptics, Dr. Beiko said. The 23-gauge forceps he uses to externalize and manipulate the haptics have blunt ends; some surgeons use forceps with ridges on the ends, he said.
The Yamane technique requires a special type of 30-gauge needle with thin walls and a wide lumen, Dr. Hannush said. (The TSK Ultra Thin Wall Needle is manufactured in Japan and distributed by Delasco.)
Geometry matters. The surgeon performing a Yamane fixation lacks tools to assure that the intrascleral tunnels are precisely equal in length (with 20-degree angulation and 5-degree tilt) and that sclerotomy entry occurs in the right places, 180 degrees apart, Dr. Fram said. “These are hard things to standardize,” and this might help explain the IOL tilt problem in Yamane eyes, she said.
Visualization. “With the glued IOL technique, you are able to directly visualize everything, at every step,” Dr. Fram said. In contrast, “with the Yamane [technique], you are marking, and then you’re going through the conjunctiva, through Tenon’s, and through the sclera—and you’re doing it blind.”
Consequently, although the Yamane technique does not call for taking down the conjunctiva, sometimes it will be helpful to do a small peritomy, about 2 clock hours, for better visualization of the sclera, she said.
Shorten the haptics. In Yamane eyes, Dr. Hannush said he has learned from experience to clip off the haptic tips before making the flanges. “Sometimes the lens will rotate in the eye if I keep them long.” Instead, he recommended, “After the IOL is centered, an asymmetric amount of haptic is clipped off, as is deemed necessary by the surgeon, thus allowing continued good centration of the lens when the 2 haptics are tucked back into the sclera.”
Glue or sutures? Some surgeons modify Dr. Agarwal’s original technique by holding the scleral flap in place with a suture instead of fibrin glue, but Dr. Beiko recommends using the glue. “The main advantage of the glue is that it decreases the postoperative inflammation. It’s not so much for stabilization of the haptic. The eyes seem to be much quieter when you don’t use sutures.”
Avoiding haptic loss. After externalizing the leading haptic during a glued procedure, the surgeon must begin externalizing the second haptic. To keep the first haptic from moving, Dr. Beiko said he devised a simple solution: He takes a tiny silicone ring (a “tire”) from an iris hook and threads the ring onto the haptic. “I’ve found this makes the fixation procedure easier for me, because it stops the haptic from slipping back into the eye.”
Final note. “With either technique, it may be a good idea to place 1 or 2 peripheral iridectomies to prevent reverse pupillary block,” Dr. Hannush said.
 |
|
TILT. Some surgeons have experienced IOL tilt with the Yamane technique.
|
___________________________
1 Hannush SB. Sutured posterior chamber intraocular Lenses. Focal Points. San Francisco: American Academy of Ophthalmology; 2006, module 9.
2 Agarwal A et al. J Cataract Refract Surg. 2008;34(9):14331438.
3 Yamane S et al. Ophthalmology. 2014;121(1):61-66.
4 Yamane S et al. Ophthalmology. 2017;124(8):1136-1142.
5 Kobori A et al. The 39th Annual Meeting of the Japanese Society of Ophthalmic Surgery, 2016.
___________________________
Dr. Beiko is in practice in St. Catharines, Ontario; a lecturer in the Department of Ophthalmology & Vision Sciences at the University of Toronto; and an associate clinical professor at McMaster University in Hamilton, Ontario, all in Canada. Relevant financial disclosures: Alcon: Nondisclosure Agreement; Bausch + Lomb: C,S; Carl Zeiss: C; Eyekon: Nondisclosure Agreement; Glaukos: C; Infinite Vision: C; Johnson & Johnson Vision: C,S; Labtician: S; Ophtec: L.
Dr. Fram is in practice with Advanced Vision Care in Los Angeles, and a clinical instructor at the Jules Stein Eye Institute at the University of California, Los Angeles. Relevant financial disclosures: None.
Dr. Hannush is attending surgeon in the Cornea Service at Wills Eye Hospital, with the Department of Ophthalmology at the Sidney Kimmel Medical College at Jefferson University, and medical director of the Lions Eye Bank of Delaware Valley, all in Philadelphia. Relevant financial disclosures: None.
See the disclosure key at www.aao.org/eyenet/disclosures.