By Jennifer E. De Niro, MD, and Rona Z. Silkiss, MD
Edited by Steven J. Gedde, MD
Download PDF
Michelle Gray* is a 51-year-old African-American woman who initially presented to a hospital emergency room with flulike symptoms and “pink eyes.” She was prescribed erythromycin ointment. Ten days later, she sought care at an ophthalmology clinic. Although her pink eye had resolved, her right upper eyelid had become diffusely swollen and was drooping. She was prescribed fluorometholone drops in case the lid swelling was due to persistent inflammation related to the conjunctivitis—but the drops failed to resolve the condition. She was referred to us for evaluation of her ptosis.
We Get a Look
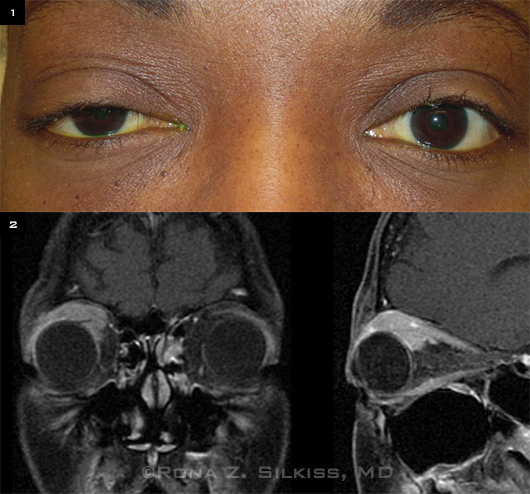
We saw Ms. Gray two weeks after her initial visit to the ophthalmology clinic. She reported that after she used the fluorometholone drops her right upper lid was no longer swollen but was still droopy. On exam, her visual acuity was 20/25 in the right eye and 20/20 in the left. Her pupils were equal in size, and there was no relative afferent pupillary defect. We noted a right superior sulcus fullness, and we could palpate an ill-defined mass in the same area. The left eyelid was normal. Hertel exophthalmometry measured 25 mm in the right eye and 22 mm in the left. Her right upper lid bisected the center of her pupil (Fig. 1). Ocular motility was intact, and IOP was normal in both eyes. The anterior segment and retinal exams were also unremarkable. She reported no medical problems, and review of systems was negative.
|
What's Your Diagnosis?
|
 |
|
WE GET A LOOK. (1) Ms. Gray demonstrates right ptosis, proptosis, and superior sulcus fullness. (2) MRI with contrast shows a confluent enhancing mass in the right superior orbit.
|
Diagnostic Results
Lab results. Complete blood count, erythrocyte sedimentation rate, thyroid panel, angiotensin-converting enzyme, lysozyme, antinuclear antibody test, and antineutrophil cytoplasmic antibodies levels, and chest x-ray were all within normal limits. MRI showed an enhancing confluent mass in the right superior orbit that was both intraconal and extraconal (Fig. 2). It measured 3.2 cm in its longest extent and encased the right superior rectus levator complex as well as the lateral rectus and lacrimal gland.
Differential diagnosis. The differential diagnosis of a diffuse intraorbital mass includes inflammatory or neoplastic lesions. Inflammatory conditions include idiopathic orbital inflammatory syndrome, lymphoid hyperplasia, infectious cellulitis, granulomatosis with polyangiitis, and sarcoidosis. Neoplastic entities include lymphoma, lacrimal gland tumors, hemangioma, and metastatic disease.
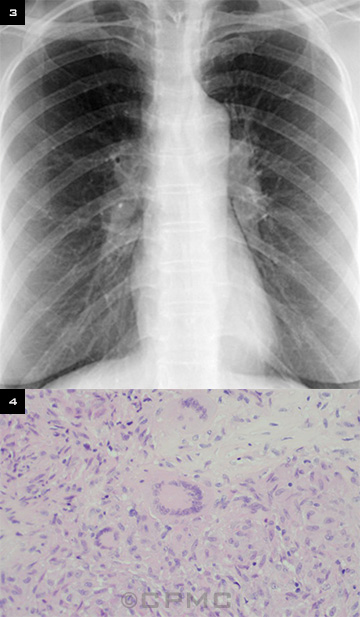
Biopsy. Ms. Gray was scheduled for an orbital biopsy. Although a chest x-ray taken three months prior was normal, a repeat x-ray the day before the biopsy demonstrated bilateral hilar adenopathy (Fig. 3). Biopsy of the orbital mass revealed granulomas that consisted of multinucleated giant cells surrounded by epithelioid histiocytes without areas of necrosis. This was consistent with sarcoidosis (Fig. 4).
Diagnosis and treatment. We made the diagnosis of orbital sarcoidosis and prescribed 40 mg of oral prednisone for one month, followed by a slow taper. Six weeks later, her ptosis and proptosis had dramatically improved, and she remained systemically well.
|
X-RAY AND ORBITAL BIOPSY. We noted (3) bilateral hilar adenopathy and (4) noncaseating granulomas.
|
Discussion
Sarcoidosis is a chronic multisystem disorder that is characterized histopathologically by noncaseating granulomas. It most frequently appears in middle age. In the United States, the annual incidence of sarcoidosis is estimated to be 36 in 100,000 for African-Americans and 11 in 100,000 for white Americans.1,2 Sarcoidosis is also more prevalent in females than in males.2 It can affect virtually any organ system, but the lungs, skin, and eyes are most commonly involved.
The most common ophthalmic manifestation is anterior uveitis. Orbital and adnexal sarcoidosis is much more rare, and only a few case series have been reported in the literature. In a retrospective case series of 30 patients with orbital and adnexal sarcoidosis, Demirci et al. found that the lacrimal gland was involved in 63 percent, the eyelid in 17 percent, the orbit in 13 percent, and the lacrimal sac in 7 percent of cases.3 Orbital and adnexal disease was unilateral in half of the cases and bilateral in the other half. Interestingly, orbital and adnexal inflammation is rarely associated with intraocular inflammation.
The diagnosis of orbital involvement in sarcoidosis patients should be based on biopsy rather than clinical findings, especially in patients who are being considered for systemic steroid or immunosuppressive therapy. Moreover, patients with an orbital mass in the presence of known systemic sarcoidosis should have an orbital biopsy because of an increased risk of malignant tumors—including malignant lymphoproliferative disease.3,4
Few studies have examined the prognostic implications of a diagnosis of orbital sarcoidosis. In the study by Demirci et al., systemic disease was diagnosed in 70 percent of the 30 patients. In 37 percent of patients, systemic disease was diagnosed before orbital and adnexal disease; in 27 percent, the diagnoses were made at the same time; and in 7 percent, the orbital and adnexal disease was diagnosed first, with a mean follow-up time of 44 months. In 30 percent of cases, no diagnosis of systemic disease was made; but according to Kaplan-Meier estimates, systemic sarcoidosis developed in 8 percent at five years.3
Systemic steroid therapy is the most common treatment for orbital sarcoidosis. Periocular steroid injections have also been used with good results.5 Fortunately, orbital sarcoidosis rarely recurs after systemic steroid therapy is tapered and stopped.3 If the orbital mass is well circumscribed and anteriorly located, it is reasonable to debulk it and opt for observation alone. Patients with orbital sarcoidosis and no systemic sarcoidosis should have long-term systemic follow-up annually by an internist or pulmonologist.
___________________________
*Patient name is fictitious.
___________________________
1 Bresnitz EA, Strom BL. Epidemiol Rev. 1983;5(1):124-156.
2 Rybicki BA et al. Am J Epidemiol. 1997;145(3):234-241.
3 Demirci H, Christianson MD. Am J Ophthalmol. 2011;151(6):1074-1080.
4 Brincker H. Sarcoidosis. 1989;6(1):31-43.
5 Mavrikakis I, Rootman J. Am J Ophthalmol. 2007;144(5):769-775.
___________________________
Dr. De Niro is a resident and Dr. Silkiss is chief of ophthalmic plastic, reconstructive, and orbital surgery; both are at California Pacific Medical Center in San Francisco. They report no related financial interests.