Download PDF
During pregnancy, the body experiences many hormonal changes that can affect the eyes. Although most of these changes are reversible and have a good prognosis, certain of these pathologies necessitate close monitoring and may require prompt management. It is important for the ophthalmologist to communicate with the patient’s obstetrician regarding ocular conditions and potential therapies.
Physiologic Changes During Pregnancy
Eyelids. One of the most common physiologic changes in pregnancy is increased pigmentation of the eyelids, known as melasma. Current research suggests that melasma results from a rise in the melanin hormone, leading to increased melanogenesis and melanocytosis. Melasma generally resolves over several months after the delivery.1
Cornea and lacrimal system. Hormonal changes during pregnancy can lead to lacrimal dysfunction and dry eye syndrome.1 Production of estrogen and progesterone are upregulated, and free serum testosterone is reduced owing to an increase in testosterone-binding protein. While testosterone promotes the development of the meibomian glands, estrogen leads to acinar cell death.
Moreover, dehydroepiandrosterone (DHEA) is reduced by 50% during pregnancy. DHEA is a major adrenal androgen that helps to maintain the structure and function of the meibomian and lacrimal glands.2
In addition to dryness, corneal sensitivity can be decreased, possibly secondary to increased corneal fluid retention.3 As a result, contact lens wear may become more difficult or even risky during pregnancy.1
Refractive considerations. Corneal thickness and curvature are increased in the second and third trimesters, likely due to water retention. Because of these changes, refractive corneal surgery is contraindicated during pregnancy. Moreover, lacrimal dysfunction complicates the recovery process after any corneal refractive procedure, as dry eye can lead to poor wound healing. Therefore, all keratorefractive surgeries such as LASIK—or even a change of prescription glasses—should be delayed until three to six months after the delivery, when the refraction has stabilized.1,4,5
Intraocular pressure. IOP has been reported to drop by 2 to 3 mm Hg during pregnancy. Although the exact mechanism behind this decrease is not established, there are several proposed hypotheses: increased aqueous humor outflow, greater tissue elasticity and subsequently lower scleral rigidity, decreased systemic vascular resistance leading to reduced episcleral venous pressure, and global acidosis in pregnancy.
The IOP often returns to prepregnancy baseline in the postpartum period. However, in patients with glaucoma, the clinical course can be variable and should be monitored.4
Pathologic Changes During Pregnancy
The conditions discussed below have the potential to cause serious ocular or systemic manifestations in the pregnant patient. Some may persist or recur after pregnancy. Thus, they warrant close monitoring and, as appropriate, coordination with specialists such as endocrinologists or rheumatologists.
Preeclampsia and Eclampsia
Preeclampsia is a form of constrictive vasculopathy that causes hypertension with either end-organ dysfunction or proteinuria. Eclampsia is the development of seizures in a patient with preeclampsia.
Ocular complications occur in about 25% to 33% of women with preeclampsia and in 50% of those with eclampsia. Patients with ocular manifestations of preeclampsia or eclampsia may experience blurred vision, scotoma, photopsia, dyschromatopsia, diplopia, transient bilateral loss of vision, and cortical blindness. Most of these visual changes are reversible and resolve in the postpartum period.1,6
Retinopathy. The most common ocular finding in preeclampsia or eclampsia is retinopathy. This type of retinopathy most commonly presents with focal narrowing of retinal arterioles, retinal edema, exudates, and hemorrhage. Occasionally, infarcts in the nerve fiber layer and vitreous hemorrhage secondary to neovascularization are seen.
Severe cases may present with retinal edema, serious exudative retinal detachment, papilledema, and acute ischemic optic neuropathy. Generally, the severity of preeclampsia dictates the degree of retinopathy.1,4
Cortical blindness. Another ocular complication of severe preeclampsia or eclampsia is cortical blindness, which occurs in 1% to 15% of cases.6 Vision loss usually occurs in the setting of an otherwise normal ophthalmologic exam and pupillary response. It is hypothesized that vasospasm leads to transient ischemia, cytotoxic edema, and transient vision loss. Although most cases of cortical blindness resolve, residual visual field defects may persist. This complication can occur both before and after delivery, and it is often accompanied by headache, hyperreflexia, and paresis.
Central Serous Chorioretinopathy
The overall annual incidence of central serous chorioretinopathy (CSC) is estimated to be 0.01%. For pregnant women, this number drops to 0.008%.7 CSC in pregnancy occurs most often in the third trimester. These patients often present with vision loss, central scotoma, delayed recovery after photostress, metamorphopsia, and loss of color saturation.
The exact pathophysiology is unknown. However, it is hypothesized that choroidal vasculopathy and abnormal ion transfer across the retinal pigment epithelium lead to serous subretinal exudation and retinal pigment epithelium detachment (Fig. 1). OCT is often the diagnostic imaging modality of choice.
CSC often resolves about three months after delivery, even without treatment. However, it can recur in the same eye in subsequent pregnancies.1
 |
|
CENTRAL SEROUS CHORIORETINOPATHY. (1A) Fundus photograph of an eye with CSC shows subretinal fluid in the macula. (1B) OCT view of subretinal fluid.
|
Occlusive Vascular Disorders
Pregnancy is known to be a hypercoagulable state that increases the risk of some ocular pathologies such as retinal artery and vein occlusions, with artery occlusion being more common. Both conditions can present as painless monocular vision loss.1
Purtscher-like retinopathy. Purtscher-like retinopathy often presents with severe bilateral vision loss shortly after the delivery. The fundus exam shows cotton-wool spots with or without intraretinal hemorrhages. These changes can resolve over time. Rarely, evidence of central or branch retinal artery occlusion and retinal vein occlusion is present. The retinopathy is associated with preeclampsia, childbirth, pancreatitis, and amniotic fluid emboli, all of which can cause arteriolar occlusion.4
Antiphospholipid syndrome (APS). APS is a hypercoagulable state that can lead to recurrent arterial and venous thrombosis and multiple miscarriages. Ocular manifestations can involve both the anterior and posterior segments.
Anterior segment involvement includes episcleritis, conjunctival telangiectasias, conjunctival microaneurysms, and iritis.
Posterior segment involvement includes vitritis, retinal hemorrhage, retinal detachment, CSC, cotton-wool spots, posterior scleritis, branch and central retinal vein occlusion, cilioretinal artery occlusion, venous tortuosity, and even bilateral choroidal infarction. Occasionally, patients present with transient vision loss (monocular or binocular), transient visual field defect, progressive optic nerve atrophy, thrombosis in ocular motor nerve, and ischemic optic neuropathy.1,4
Disseminated intravascular coagulation (DIC). DIC is a disorder of blood-clotting proteins that can be associated with various conditions such as inflammation, infection, and cancer as well as pregnancy. When it occurs in pregnancy, it is secondary to a variety of obstetric complications such as amniotic fluid embolism, preeclampsia/eclampsia, intrauterine fetal death, placental abruption, septic abortion, intrauterine infection, acute fatty liver disease of pregnancy, or placenta previa.
DIC often affects the choroid. This hypercoagulable state can lead to thrombus formation in the choriocapillaris and subsequent disruption of retinal pigment epithelium, which can result in development of serous retinal detachment.1,4
Sheehan Syndrome
Sheehan syndrome is ischemic pituitary necrosis and pituitary gland enlargement secondary to severe postpartum hemorrhage. The common presentation includes sudden headache, vision loss, visual field defect, and ophthalmoplegia. The visual field defects usually involve the loss of bitemporal superior quadrant fields.
Compression of the cavernous sinus leads to compression of cranial nerves III, IV, and VI, which can manifest as ptosis, diplopia, lateral-inferior deviation of the globe, and mydriasis. If sympathetic nerve fibers are involved, Horner syndrome may be present as well. Vision improvement is less likely than improvement of the ophthalmoplegia.4
 |
|
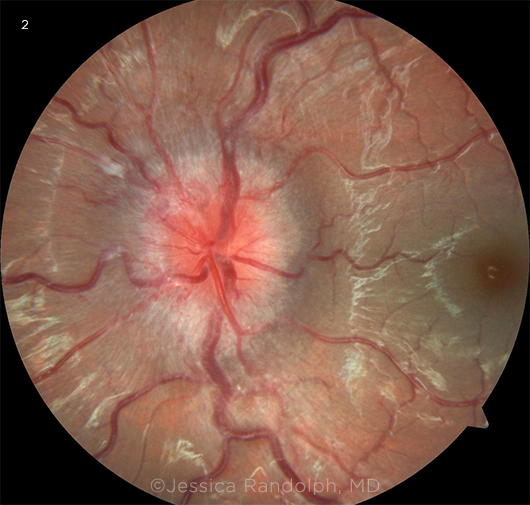
IDIOPATHIC INTRACRANIAL HYPERTENSION. Fundus photograph shows optic nerve with disc edema from IIH. Note the obscuration of the disc margins.
|
Idiopathic Intracranial Hypertension
Idiopathic intracranial hypertension (IIH, Fig. 2) is most commonly seen in obese females of childbearing age. When it occurs during pregnancy, it most often presents in the first trimester. IIH causes headaches as well as a variety of visual symptoms such as diplopia, visual field defect, scotoma, photopsia, retrobulbar pain, and pulsatile tinnitus. Although the fundus exam reveals bilateral papilledema in most cases, some patients may present with unilateral or no papilledema.1,4
The diagnosis of IIH is one of exclusion, characterized by elevated opening pressure, but normal brain imaging, cerebrospinal fluid composition, and neurologic exam.8 Medical treatment focused on lowering the intracranial pressure and postpartum weight loss are recommended.1,5 Pregnant patients may be treated with acetazolamide, optic nerve sheath fenestration, lumboperitoneal shunt, or ventriculoperitoneal shunt. Although acetazolamide showed teratogenicity in animal studies, recent studies on pregnant women found no increased risk to the fetus or the mother, and it can be considered a treatment option. There are no modifications or limitations to delivery method based on a diagnosis of IIH, and the decision should be made between the patient and her obstetrician.9
Graves Disease
Graves disease is the most common cause of hyperthyroidism during pregnancy. The disease often manifests as unilateral or bilateral proptosis, lid lag, and extraocular muscle palsies. Graves disease most commonly occurs in the first trimester, followed by remission in the second and third trimesters. Although the mild cases are often managed by monitoring, moderate to severe cases may require medical management with propylthiouracil.4 Teprotumumab is contraindicated during pregnancy.
Pituitary Tumors
The fast growth of preexisting pituitary tumors during pregnancy most likely occurs as a result of the angiogenic effect of estrogen. This growth leads to intracranial space–occupying symptoms such as compressive optic chiasm/tract neuropathy. The most common presentations are decreased visual acuity, bitemporal visual field defect, and diplopia. In patients with preexisting pituitary adenoma, monthly visual field and ophthalmologic exam are needed to monitor adenoma growth.4
 |
|
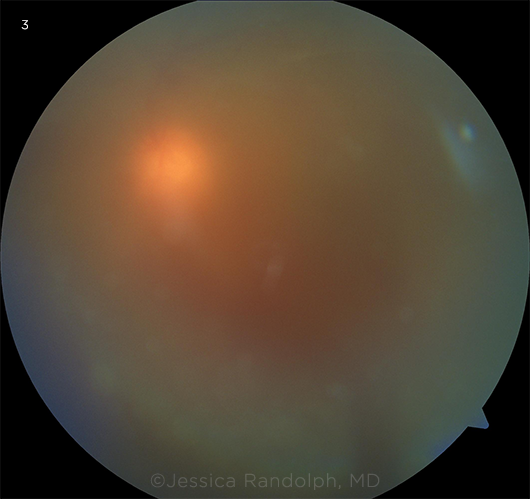
UVEITIS. Fundus image of a patient with vitritis demonstrates the hazy view to the posterior pole. The nerve is barely visible through the vitreous cells.
|
Preexisting Ocular Disease
Diabetic retinopathy. Current evidence indicates that diabetic retinopathy can develop and progress during pregnancy. The progression of retinopathy is affected by the duration of diabetes, degree of retinopathy before pregnancy, glycemic control, and presence of other comorbidities such as hypertension.1,4
The Academy’s Comprehensive Adult Medical Eye Evaluation Preferred Practice Pattern guidelines recommend that all women with diabetes should have a fundus exam prior to conception and during the first trimester. The frequency of follow-up during the second and third trimesters is dictated by the severity of retinopathy.4 For women with severe nonproliferative retinopathy, a fundus exam is recommended every two to three months. Women with proliferative disease need more frequent monitoring.1
In patients with proliferative and severe nonproliferative disease before pregnancy, panretinal laser photocoagulation could lower the risk of disease progression by 50%. Panretinal photocoagulation is safe to administer during the pregnancy. Additionally, diabetic macular edema may worsen during the pregnancy but often resolves spontaneously postpartum. In rare cases, edema may persist after the pregnancy and lead to long-term visual defects. Although anti-VEGF injections are the main treatment of macular edema and neovascularization, they are usually avoided in pregnancy.10
Currently, no clinically significant correlation has been identified between gestational diabetes and diabetic reti-nopathy development. Therefore, women with gestational diabetes do not require regular eye exams during pregnancy.4
Uveitis. Cases of noninfectious uveitis (Fig. 3) often improve in the second or third trimester of pregnancy, although the underlying mechanism is unclear. This altered immune response may allow for tapering of immunosuppressive medications during pregnancy.4
Many commonly used immunosuppressive medications are contraindicated in pregnancy, as they can cause fetal abnormalities. The most important medications to avoid during pregnancyare mycophenolate, methotrexate, leflunomide, and cyclophosphamide. However, low-dose steroids, hydroxychloroquine, cyclosporine, azathioprine, sulfasalazine, and tumor necrosis factor blockers such as infliximab, certolizumab, and adalimumab are considered safer.
There are not yet enough data on the safety of some biologics such as rituximab and tocilizumab. Thus, they should be avoided during pregnancy. It is critical for patients to have detailed discussions with their obstetrician and rheumatologist about the choice of immunosuppressive medication prior to pregnancy.11
Toxoplasmosis. Reactivation of latent ocular toxoplasmosis may occur in pregnancy; it can lead to symptoms in the mother and congenital infection in the child. In immunocompetent patients, toxoplasma retinochoroiditis is the most common cause of posterior uveitis. In active cases, retinal necrosis, vasculitis, vitritis, and choroiditis may be present. These cases typically present as the “headlight in the fog” finding on fundus examination (Fig. 4). In rare cases, neuroretinitis, papillitis, scleritis, and Fuchs-like anterior uveitis and retinal necrosis have been reported as well.4
Active infection during pregnancy is treated with oral spiramycin or pyrimethamine-sulfadiazine with folinic acid until delivery to decrease maternal transmission to the fetus.12 Intravitreal clindamycin and dexamethasone can also be used as adjuvant therapy.4
 |
|
TOXOPLASMOSIS. Fundus photo shows the “headlight in the fog” appearance and an inferotemporal area of retinal whitening at the edge of the image.
|
Conclusion
Many physiologic and pathologic ocular changes can occur during pregnancy. Major physiologic changes include melasma, refractive changes, lacrimal gland dysfunction, and temporary decrease in IOP. Most of these effects resolve spontaneously after the delivery. Additionally, pregnancy can lead to pathologic conditions such as retinopathy, CSC, occlusive vascular disorders, Sheehan disease, IIH, Graves disease, and pituitary tumors. Finally, preexisting eye conditions such as diabetic retinopathy, uveitis, and toxoplasmosis can present challenges in pregnant women and may require consultation with specialists.
___________________________
1 Rezai S et al. Obstet Gynecol Int J. 2016;4(1):00093.
2 Nkiru Z N et al. Ocul Surf. 2019;17(3):458-463.
3 Riss B, Riss P. Ophthalmologica. 1981;183(2):57-62.
4 Naderan M. J Curr Ophthalmol. 2018;30(3):202-210.
5 Bower KS, Woreta F. Curr Opin Ophthalmol. 2014;25(4):251-257.
6 Abu Samra K. Saudi J Ophthalmol. 2013;27(1):51-53.
7 Kra ANS et al. Open J Ophthalmol. 2018;08(04):207-213.
8 Friedman DI et al. Neurology. 2013;81(13):1159-1165.
9 Kesler A, Kupferminc M. Clin Obstet Gynecol. 2013;56(2):389-396.
10 Naderan M et al. Int Ophthalmol. 2021;41(2):743-751.
11 Agrawal H et al. Indian J Ophthalmol. 2020;68(9):1852-1862.
12 Maldonado YA, Read JS; Committee on Infectious Diseases. Pediatrics. 2017;139(2):e20163860.
___________________________
Dr. Ataei is a PGY1 at Medical College of Wisconsin Affiliated Hospitals and Dr. Randolph is an assistant professor and vitreoretinal surgeon in the department of ophthalmology at Virginia Commonwealth University, Richmond, Va. Financial disclosures: None.