By Ahmad A. Aref, MD, MBA, with Albert S. Khouri, MD, and Constance O. Okeke, MD, MSCE
Download PDF
Microinvasive glaucoma surgeries, or MIGS, constitute a broad array of devices and procedures for managing glaucoma. In this first portion of a two-part series, Ahmad Aref, MD, MBA, of the University of Illinois in Chicago, hosts an MD Roundtable with Constance O. Okeke, MD, MSCE, of Virginia Eye Consultants in Norfolk, and Albert S. Khouri, MD, of Rutgers New Jersey Medical School in Newark. The experts discuss how they define and categorize MIGS, their thought processes for selecting a particular procedure, and when they consider employing a “MIGS-plus” modality. Part 2 will appear in the November EyeNet.
Defining MIGS
Dr. Aref: How do you define MIGS?
Dr. Okeke: MIGS are microinvasive glaucoma surgeries. In the past, we called these types of surgeries “minimally invasive.” The microinvasive terminology refers to the lack of conjunctival tissue disruption and the ab interno nature of the approach through a clear corneal incision to access the angle structures. Usually, MIGS address the conventional outflow pathway, but they also can involve the uveoscleral pathway. Compared with traditional glaucoma surgeries, MIGS are thought to be less traumatic and to have better efficiency in terms of time in the OR and post-op healing.
Dr. Khouri: I think the term “microinvasive” is appropriate to reflect the good safety profile and less burdensome post-op period associated with MIGS, compared with traditional glaucoma surgery. I also like to use the phrase “precision glaucoma surgery,” which reflects how MIGS enable us to be much more precise in tissue handling.
Ciliary Body MIGS
Dr. Aref: Do you consider procedures that ablate the ciliary body—specifically endoscopic cyclophotocoagulation (ECP) and the MicroPulse laser system (Iridex)—within the scope of MIGS?
Dr. Okeke: An incision needs to be made to perform ECP; so yes, I consider it to be a microinvasive, or microincisional, glaucoma surgery. The MicroPulse system does not involve an incision, so I think of it as a laser tool rather than as part of the MIGS array.
Dr. Khouri: I find it challenging to place surgical procedures in specific categories because it depends on how we use them. ECP and MicroPulse both have relatively good safety profiles, and they’re less invasive than traditional glaucoma surgeries. MicroPulse is a laser surgical intervention with broad applications for managing moderate to advanced or refractory glaucoma. In a way, MicroPulse fits the definition of MIGS, but not entirely.
Dr. Aref: I agree. I think these ciliary body procedures can be distinguished from other MIGS by the expanded range of glaucoma stages that can be treated.
Choosing a Procedure
Dr. Aref: What is your thought process for selecting MIGS procedures?
Dr. Okeke: I use somewhat of an algorithm in MIGS selection. I first want to get a sense of the kind of glaucoma. For this, I evaluate the angle anatomy, so gonioscopy is crucial for helping me decide what kind of MIGS procedure to use. I check whether the angle is open, and I also look for characteristics of secondary glaucoma, such as pseudoexfoliation, increased pigment, or angle recession. I have found that a goniotomy procedure with the Trabectome (NeoMedix) tends to work well in patients with pseudoexfoliation glaucoma.1 I also check for signs of uveitis, synechiae, and appositional closure of the angle.
With angle recession, the anatomic location of the recession is important. Typically, I want to address the nasal quadrant, and if angle recession is significant there, I would expect that the outflow system isn’t functioning well. Therefore, I wouldn’t be confident that goniotomy or a stenting procedure in that area would yield good results.
In addition, the glaucoma stage weighs into MIGS selection. Is the patient on just one medication and in need of a procedure to get off that medication and remain stable? Does the patient have more advanced glaucoma treated with several medications? In the latter case, I would want to use a more robust device, like a Xen gel stent (Allergan), which is placed subconjunctivally.
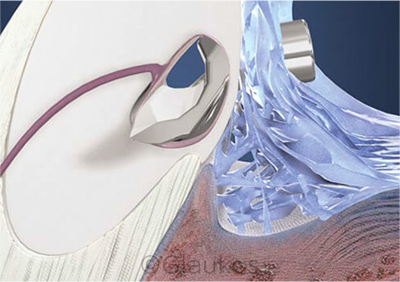
I also evaluate the patient for cataract. Some MIGS must be done in combination with cataract surgery, and there are other MIGS that can be done alone, such as goniotomy and canaloplasty. For example, in a patient with early glaucoma and no cataract, a stenting procedure—such as with the iStent or iStent inject (both, Glaukos)—would not be suitable.
If the patient has had previous laser therapy—say, selective laser trabeculoplasty (SLT)—I’ll review the medical record to find out whether it was successful. If it was, then I would expect the patient to benefit from procedures that promote trabecular meshwork outflow, such as goniotomy, stenting, or potentially canaloplasty.
I also give thought to which procedures will be covered by the patient’s health insurance. It’s important to consider those practical concerns as well.
Dr. Khouri: When I’m deciding among MIGS options, I perform extensive gonioscopy. I want to examine the angle and look for appositional or synechial closure.
There has been an explosion in the use of MIGS, and these procedures are approved primarily for open-angle glaucoma, based on data from clinical trials.2 However, we encounter diverse clinical situations in glaucoma management, and as we gain experience applying these technologies to best care for patients, our use of MIGS may gradually change.
In recent studies, MIGS have been applied to treat more advanced and even refractory glaucoma with somewhat favorable results. For instance, Neuhann3 found a 36% reduction in mean intraocular pressure (IOP) after iStent placement plus cataract surgery in a group of patients with varied disease severity, including some with advanced glaucoma. In a retrospective review of 42 eyes with severe glaucoma, phacoemulsification was combined with the Kahook Dual Blade (New World Medical) and was found to lower IOP to ≤15 mm Hg by six months post-op in approximately two-thirds of eyes.4 Angle surgery to treat appositional angle closure also seems to work well. Bussel and colleagues5 demonstrated that ab interno trabeculectomy with the Trabectome significantly decreased pressure in eyes with narrow angles.
There’s still a lot we don’t know about the effects of MIGS in certain settings, such as in patients who were on particular medications previously or who had received laser treatment. At this year’s annual meeting of the American Glaucoma Society, my colleagues and I presented findings of a two-center retrospective study of 91 patients who underwent trabecular bypass with an iStent.6 We showed that the group of patients who received previous laser trabeculoplasty had less pronounced reductions in IOP and in number of medications needed than did patients without prior laser therapy. This was a surprising result. But we did demonstrate that the decrease from baseline in medication burden was significant in both groups. A limitation of our study was that we did not have full access to data on the response after SLT and whether that predicted the outcomes of iStent placement.
These findings emphasize that we are in a pilot phase. We still have much work to do in determining which devices work best for which patients.
Dr. Okeke: Dr. I. Paul Singh found that, in patients who underwent iStent placement, those who previously had good results with laser SLT were more likely to have success with the iStent.7 So there may be a use for SLT as an indicator. When SLT is successful, it could mean that the conventional outflow system still is functional and that other interventions to enhance outflow would likely succeed.
Dr. Aref: That’s very interesting because we don’t have a way to visualize the outflow system with regularity. SLT efficacy might be usable as a surrogate for outflow function until we have the ability to precisely measure the patency of a patient’s outflow system.
Dr. Khouri: We now also have medications that work on the trabecular meshwork—like Rho kinase inhibitors and nitric oxide—and we still are trying to figure out whether the response to those medications can also be a predictor for bypassing the meshwork. There’s a lot of work ahead for us, but it’s an exciting time for glaucoma specialists.
 |
|
ISTENT. Some patients with advanced glaucoma have shown favorable results with the iStent, according to a 2015 study by Neuhann.3
|
MIGS-Plus
Dr. Aref: The Xen implant is considered a MIGS-plus device; how does it differ from the other MIGS modalities we’ve discussed?
Dr. Okeke: In its classic form, the Xen implant is placed through an ab interno approach, and mitomycin C is delivered under the conjunctiva. This conjunctival disruption isn’t as substantial as with traditional glaucoma surgery, but it does involve slightly more risk than do typical MIGS procedures.
In addition, patients who receive the Xen implant may require needling to revise the conjunctival bleb, which increases the complexity and risk of this procedure. Early data from the FDA registration trial8 indicated that about one-third of patients required needling (21 of 65 patients; 32.3%). MIGS are being adopted by glaucoma specialists and by comprehensive cataract surgeons. And with the Xen implant, one needs to understand and be comfortable with the possibility of needling during follow-up.
Some practitioners have started using an ab externo Xen approach, which still is less invasive than traditional trabeculectomy in terms of manipulating the conjunctiva. The ab externo approach may help decrease the post-op risk of needling, but again, the intra- and post-op risk associated with mitomycin C delivery remains.
Dr. Aref: I think it’s important to consider that the patients in the FDA registration trial had some unique characteristics. These patients had failure of previous filtering or cilioablative procedures or had uncontrolled IOP on maximal medical therapy.8
Dr. Khouri: The way in which patients heal is crucial for the success of MIGS and MIGS-plus procedures. This healing process can be unpredictable and varies by age and ethnicity. Therefore, patient selection is key, and patients should be informed that healing can affect their surgery’s outcome.
I would include the Xen device in a category of precision glaucoma surgeries. Compared with conventional trabeculectomy, Xen placement involves a much smaller incision, less manipulation of the tissue, and less reliance on suturing and technique. However, with any subconjunctival surgery, certain patient groups with vigorous healing can have unsatisfactory results. These include patients who are younger, Hispanic people, and those of African origin. Patients who’ve undergone ocular surgery or conjunctiva manipulation also tend to be “primed” to heal more aggressively. In addition, those on maximal therapy for a prolonged period tend to have chronic conjunctival inflammation and robust healing after Xen implantation.
Discussions with the patient are vital; he or she must be prepared to deal with potentially burdensome post-op care, similar to that of conventional trabeculectomy. The rates of needling do seem to be lower with the Xen stent than with trabeculectomy. When a favorable bleb forms after Xen, the IOP reductions are comparable to trabeculectomy, and this is important for patients with advanced glaucoma. Notably, the FDA registration trial of the Xen stent included only one-year data.8 In high-risk populations, the needling rates may be higher than 30%—and in some patients, the treatment will fail. In other words, the healing can be so vigorous as to require multiple needling sessions after Xen implantation and may still result in scar formation and the need for additional surgery. Patients with this outcome typically have more advanced glaucomatous disease and lower target pressures. All these factors come into play as we select which procedure will work best for the patient.
Dr. Aref: That’s the art of glaucoma: individualizing our care.
___________________________
1 Okeke CO et al. Medicine (Baltimore). 2017;96(24):e7061.
2 Lavia C et al. PLoS One. 2017;12(8):e0183142.
3 Neuhann TH. J Cataract Refract Surg. 2015;41(12):2664-2671.
4 Hirabayashi MT et al. Clin Ophthalmol. 2019;13:715-721.
5 Bussel II et al. Br J Ophthalmol. 2015;99(7):914-919.
6 Bargoud A et al. Presented at AGS 2019 Annual Meeting; San Francisco; March 14-17, 2019.
7 Personal communication from I. Paul Singh, MD, July 31, 2019.
8 Grover DS et al. Am J Ophthalmol. 2017;183:25-36.
___________________________
Dr. Aref is associate professor of ophthalmology at the University of Illinois in Chicago. Relevant financial disclosures: New World Medical: C.
Dr. Khouri is associate professor of ophthalmology at Rutgers New Jersey Medical School in Newark. Relevant financial disclosures: Allergan: L,S; Glaukos: C.
Dr. Okeke is a glaucoma specialist at Virginia Eye Consultants and assistant professor of ophthalmology at Eastern Virginia Medical School in Norfolk. Relevant financial disclosures: Allergan: C; Ellex: C,L; Glaukos: C,L,S; NeoMedix: L; Santen: C; Sight Sciences: C.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Aref Aerie: L; New World Medical: C.
Dr. Khouri Aerie: C,L; Bausch + Lomb: L; Allergan: L,S; Glaukos: C; New Jersey Health Foundation: S.
Dr. Okeke Aerie: C,L; Allergan: C; Bausch + Lomb: C,L; Ellex: C,L; Glaukos: C,L,S; Kugler Publications: P; NeoMedix: L; Novartis (Alcon): C; Reichert: L; Santen: C; Sight Sciences: C.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|