By John Deans, MD, Kathy Whitfield, MD, Alice Yang Zhang, MD, and Kenneth L. Cohen, MD
Edited By: Ingrid U. Scott, MD, MPH
Download PDF
Jennie Davis,* a 15-year-old with a history of cystic fibrosis, had been experiencing progressive decreased vision and difficulty with her night vision in both eyes for almost three years.
After seeing her primary care physician, she was referred to our clinic for evaluation.
We Get a Look
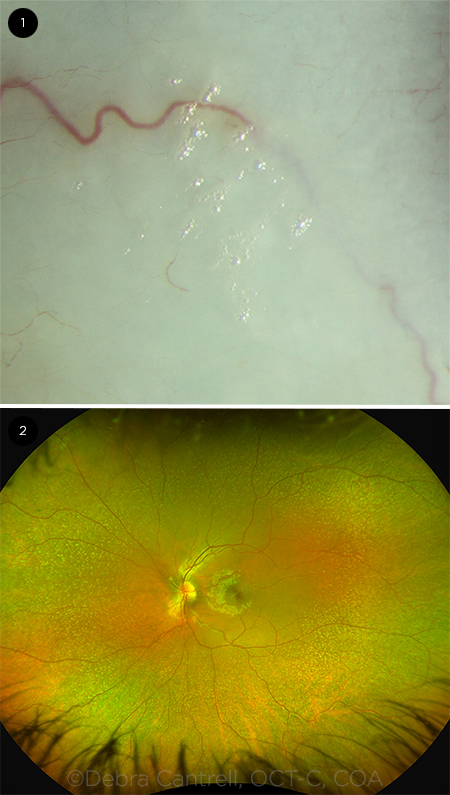
When we examined Jennie, her best-corrected visual acuity was 20/40 in her right eye and 20/50 in her left. In both eyes, intraocular pressure was normal, and color vision was 11/11 in each eye on testing with Ishihara plates. The anterior segment exam was notable for areas of dryness and early foamy plaques on the conjunctiva bilaterally (Fig. 1).
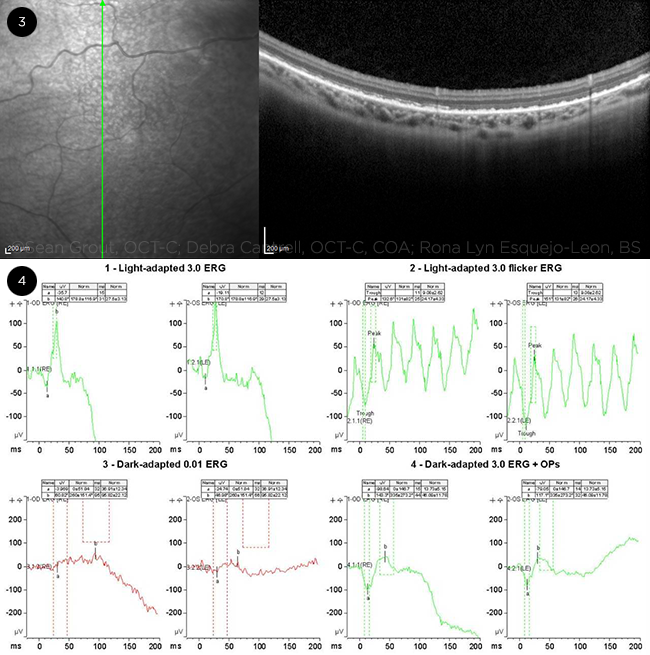
The dilated ophthalmoscopic exam showed a normal-appearing optic nerve and macula in both eyes, but both retinas had innumerable yellow-white punctate deposits which appeared deep to the retina and were more pronounced in the periphery (Fig. 2).
 |
|
WE GET A LOOK. (1) When we performed the slit-lamp examination, plaques of foamy spots were visible on both conjunctivas. (2) The dilated ophthalmoscopic exam was note- worthy for numerous yellow-white dots in both retinas, particularly in the periphery.
|
Further Investigations
We further reviewed Jennie’s medical and surgical history. It included cystic fibrosis–related pancreatic insufficiency, for which she was receiving standard enzymatic replacement therapy. As a neonate, she had developed meconium ileus, which necessitated multiple bowel resections, resulting in short gut syndrome. Two years prior to our evaluation, she had received a liver transplant for unspecified liver disease. Her clinical course was complicated by low-level chronic rejection.
The yellow-white deposits in Jennie’s peripheral retina raised concerns for a fleck retina syndrome. Macular optical coherence tomography (OCT) was performed, showing multiple subretinal deposits with photoreceptor disruption (Fig. 3). Electroretinography (ERG) demonstrated a decreased scotopic response (Fig. 4).
 |
|
FURTHER INVESTIGATIONS. When developing our differential, we ordered OCT and an ERG. (3) Macular OCT reveals subretinal deposits and photoreceptor disruption. (4) ERG tracings demonstrate a decreased scotopic response.
|
Differential Diagnosis
The differential diagnosis of nyctalopia includes common disorders such as uncorrected myopia, cataract, and glaucoma.
Congenital or genetic conditions can also be implicated. These include retinitis pigmentosa, congenital stationary night blindness, Oguchi disease, choroideremia, gyrate atrophy, or ocular albinism.
Other acquired causes of nyctalopia include vitamin A deficiency, zinc deficiency, medications such as thioridazine or chloroquine, siderosis, or a history of panretinal photocoagulation.
Our Diagnosis
Given the findings of xerosis and fleck retinopathy, in combination with Jennie’s history of cystic fibrosis with pancreatic insufficiency and short gut syndrome, we placed vitamin A deficiency at the top of our differential.
We obtained serum vitamin A levels, which measured <5 μg/dL (the reference range for individuals who are 13-17 years old is 14.4-97.7 μg/dL), confirming the diagnosis of vitamin A deficiency.
Discussion
Vitamin A consists of a group of lipid-soluble compounds known as retinoic acids. Along with the other fat-soluble vitamins D, E, and K, vitamin A must be acquired through the diet or supplementation. These compounds undergo emulsification by bile salts in the duodenum and absorption in the ileum before being stored in the liver or adipose tissue.
Vitamin A has essential functions in phototransduction, cellular differentiation, epithelial maintenance, and immunity. Although vitamin A deficiency is commonly associated with malnutrition, our patient’s case highlights the fact that this condition is not confined to developing nations. Rather, it can occur in any patient with liver, gallbladder, pancreatic, or small-bowel pathology that impairs vitamin A absorption, despite an adequate dietary intake.
Etiology and Epidemiology
Vitamin A deficiency is the leading cause of preventable childhood blindness worldwide. The World Health Organization estimated that in 2013, the deficiency affected approximately one-third of children aged 6-59 months, with higher rates in sub-Saharan Africa (48%) and South Asia (44%).1
In the developed world, vitamin A deficiency is much rarer but may occur in fat malabsorption conditions such as cystic fibrosis, celiac disease, primary biliary cirrhosis, small-bowel Crohn’s disease, and short gut syndrome, as well as after bariatric surgery. It may also be seen with hepatic cirrhosis, most commonly due to alcoholism, and in patients following severely restricted diets by choice or as a result of mental health conditions.
What the Ophthalmologist Should Look For
Nyctalopia is the earliest and most common symptom of vitamin A deficiency. This occurs due to an insufficient supply of the chromophore 11-cis retinal, which is a derivative of vitamin A and a necessary constituent of the visual pigment rhodopsin.
The next ophthalmic manifestation is conjunctival and corneal xerosis. In the absence of vitamin A, which has vital functions in epithelial maturation, there is a loss of mucin-secreting conjunctival goblet cells. This will result in tear film disruption and dryness. Bitot’s spots are a classic associated finding (see the foamy spots in Fig. 1). These triangular patches of xerosed conjunctiva represent areas of squamous metaplasia with overlying keratin debris mixed with Corynebacterium xerosis. The gas that is produced by this bacterium accounts for the foamy appearance of these lesions.
Finally, vitamin A deficiency can cause a fleck retinopathy, as shown in Figs. 2 and 3. The cause and composition of these small, white peripheral subretinal dots is not yet known, but they may represent areas of photoreceptor damage or lipofuscin accumulation.2
Complications
The xerophthalmia associated with vitamin A deficiency represents a spectrum of disease. The earliest findings of conjunctival dryness with Bitot’s spots and corneal punctate epithelial erosions may progress to peripheral corneal ulcers or keratomalacia with full-thickness liquefactive necrosis of the cornea. Blindness may result from scar formation and/or corneal decompensation.
Confirming the Diagnosis
Vitamin A deficiency is a clinical diagnosis; however, additional testing may be beneficial for confirmation. For adults, a serum vitamin A level of <30 μg/dL is suggestive but not diagnostic, as serum levels do not fully reflect hepatic vitamin A stores and may be depressed in protein-deficiency states.1,3 Retinol-binding protein (RBP) levels may also be measured. The reference range is 30 to 75 mg/L, and a serum retinol:RBP ratio of <0.8 suggests vitamin A deficiency. Conjunctival impression cytology may be considered; histology shows squamous metaplasia of the conjunctival epithelium and goblet cell loss. Further evaluation of nyctalopia or xerophthalmic fundus may also include ERG, OCT, fluorescein angiography, and visual fields.
Treatment
Vitamin A deficiency is treated with high-dose oral or intramuscular vitamin A supplementation. Dose adjustments are required for infants and pregnant women.4 Topical retinoic acid (0.1%) may serve as adjunctive therapy in cases of xerosis, as healing may be delayed several days from the start of systemic therapy. Nyctalopia improves or resolves within 48 hours of treatment, and retinopathy has been shown to resolve within eight months.2
Our Patient’s Course
Jennie was referred to the nutritional services department. She was initially treated with a beta carotene–based supplement. However, this treatment did not improve her symptoms or vitamin A levels, which suggested that she could not convert beta carotene to retinol in her gut because of prior bowel resections. Therefore, her therapy was changed to retinyl palmitate, a preformed type of vitamin A. Because zinc is a necessary cofactor of RBP, she was started on zinc supplementation as well.
With the above regimen, Jennie’s serum vitamin A recovered to a normal level of 17.0 μg/dL. Her nyctalopia resolved, as did her yellow-white deposits. We performed OCT and found that her macula had normalized, but the patient did not return for repeat ERG.
Conclusion
Vitamin A deficiency is the leading preventable cause of childhood blindness worldwide, but it can also occur in the developed world in patients with fat malabsorption or liver disease.5 Ophthalmic manifestations include night blindness, xerophthalmia, and retinopathy. Treatment is oral or intramuscular vitamin A supplementation.
___________________________
*Patient name is fictitious.
___________________________
1 https://data.unicef.org/topic/nutrition/vitamin-a-deficiency. Accessed March 11, 2020.
2 Chow CC, Mieler WF. Retin Cases Brief Rep. 2014;8(3):164-166.
3 Krishna U et al. EyeNet. 2016;20(12)35-36. aao.org/eyenet/article/management-of-bitot-s-spots. Accessed Feb. 13, 2020.
4 World Health Organization. Vitamin A supplements: a guide to their use in the treatment and prevention of vitamin A deficiency and xerophthalmia. 2nd ed. 1997. www.who.int/nutrition/publications/micronutrients/vitamin_a_deficiency/9241545062/en/. Accessed Feb. 13, 2020.
5 McLaughlin S et al. Eye (Lond). 2014;28(5):621-623.
___________________________
Dr. Deans is chief resident of ophthalmology; Dr. Whitfield and Dr. Zhang are both assistant professors of ophthalmology; and Dr. Cohen is the Sterling A. Barrett Distinguished Professor Ophthalmology. All four are at the University of North Carolina at Chapel Hill. Financial disclosures: None.