By Jamie Lea Schaefer, MD, Gareth Lema, MD, PhD, and Sangita P. Patel, MD, PhD
Edited By: Steven J. Gedde, MD
Download PDF
Meg Ross*, a 47-year-old librarian, came into our clinic for follow-up of dry eye disease secondary to Sjögren syndrome. Her dry eye symptoms were under good control with artificial tears and Lacri-Lube (white petrolatum–mineral oil). She told us that her internist had recently started her on hydroxychloroquine therapy for her Sjögren syndrome. We decided to initiate baseline testing for future monitoring of hydroxychloroquine toxicity.
We Get a Look
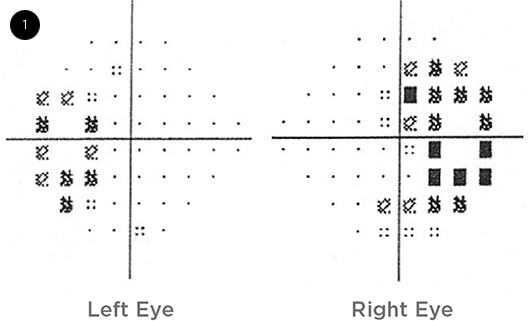
When we examined Mrs. Ross, her best-corrected visual acuity was 20/25 in the right eye and 20/20 in the left. She had full visual fields on confrontation. There was no acute disease process on the dilated fundus exam, and no changes were observed in the macula. We ordered Humphrey 10-2 visual fields to obtain a baseline for monitoring hydroxychloroquine toxicity. The Humphrey 10-2 visual field test showed bitemporal visual field defects. We then ordered Humphrey 24-2 visual fields, which confirmed bitemporal field defects (Fig. 1).
 |
|
WE GET A LOOK. When we checked the patient’s visual fields, we noticed bitemporal field defects.
|
Further Investigations
Because bitemporal visual field defects are often associated with optic chiasm lesions, especially pituitary lesions, we questioned Mrs. Ross further about any associated symptoms. She denied experiencing headaches, and a review of symptoms revealed no endocrinologic or constitutional symptoms.
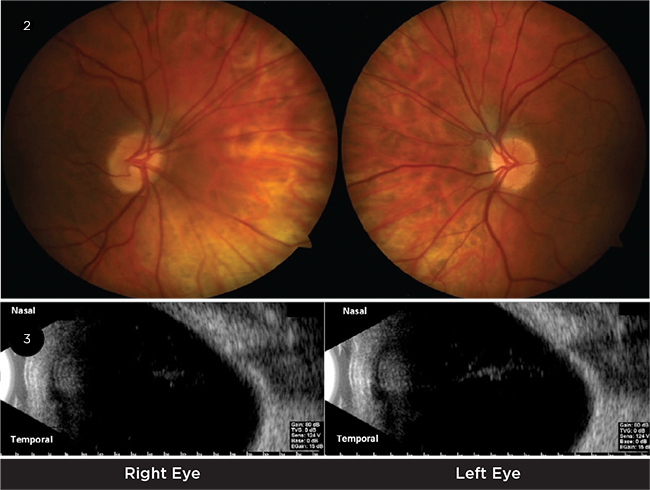
Magnetic resonance imaging (MRI) of the brain and orbits was negative for pituitary lesions or other compressive lesions involving the midoptic chiasm and thus could not explain her visual field results. We looked again at the visual field and noted that the defect crossed the vertical midline, suggesting that the origin could be anterior to the optic chiasm. On a return visit, we noted tilted insertions of the optic nerves and diffuse atrophy of the nasal retinal pigment epithelium (RPE, Fig. 2). Macular OCT was performed and normal foveal contour was noted. We verified the optic nerves’ oblique insertion by ultrasound B-scan (Fig. 3).
Differential diagnosis. The differential diagnosis of bitemporal hemianopia includes tumors causing compression at the midoptic chiasm, such as pituitary adenomas and craniopharyngiomas, and aneurysms of the anterior communicating artery. An additional cause of bitemporal visual field defects is tilted disc syndrome.
 |
|
IMAGING. (2) We observed tilted insertions of the optic nerves and diffuse atrophy of the nasal RPE. (3) Ultrasound B-scan confirmed the oblique insertion of the optic nerves.
|
Making the Diagnosis
Considering that Mrs. Ross had bitemporal visual field defects that did not respect the midline, negative imaging studies for an optic chiasmal lesion, and tilted disc insertion that was confirmed on clinical evaluation and ultrasound B-scan, we diagnosed her with tilted disc syndrome. After completing a workup for intracranial pathology, we could reassure her that this condition was anatomic, not pathologic.
Discussion
Visual field testing is performed for a variety of reasons, including mapping of defects from intracranial pathology, glaucoma monitoring, monitoring retinal toxicity from hydroxychloroquine use, and investigating unexplained visual field or visual acuity loss.
This case is important because it demonstrates the investigative steps necessary in evaluation of bitemporal visual field loss. Highest on the differential is a lesion-causing compression at the optic chiasm. However, when that is ruled out, a careful ocular exam may show the congenital anomaly of tilted disc syndrome as a cause for bitemporal visual field defect, as observed in this patient.
Etiology. Tilted disc syndrome is a congenital malformation of the optic nerve.1,2 Two accepted theories for the etiology of the syndrome include incomplete closure of the optic fissure during embryonic development at 6 weeks of gestation or hypoplasia of the inferonasal optic nerve head.
What to look for. Tilted disc syndrome can be identified by the oblique insertion and anomalous shape of the optic nerve; situs inversus of the major retinal vessels; myopic astigmatism; focal hypopigmentation; and ectasia of the inferonasal retina, RPE, choroid, and scleral layers of the globe. Mrs. Ross had previous LASIK surgery at another facility with unknown preoperative refraction. One of the most characteristic findings of tilted disc syndrome is Fuchs coloboma, an ectatic defect of the inferior and inferonasal disc. Tilted disc syndrome is predicted to occur in 1%-2% of the population, and milder forms may go undiagnosed.3 It occurs bilaterally 60%-80% of the time and is most often associated with high myopia.
Visual field defects. When tilted disc is found bilaterally, the visual field defects may mimic optic chiasm disorders.1 Axonal dysgenesis causes the visual field defects that occur with tilted disc syndrome.2 These defects generally involve the temporal and superior visual field but may appear as an enlarged blind spot. The edges of the field defects typically cross the midline of the visual field in tilted disc syndrome, whereas defects resulting from chiasmal disorders respect the true vertical hemianopic line.
Potential for myopic correction. We noted during our clinical exam that Mrs. Ross’ confrontational visual fields were full. Since bitemporal hemianopic defects may result from a refractive blind spot correlating to the ectatic fundus, these defects may often be reduced with myopic correction.4 In contrast to glaucomatous or chiasmal visual field defects, the addition of a small myopic correction (1-2 D) can improve the visual field defects of tilted disc syndrome.
Complications. Although tilted disc syndrome is considered a benign congenital anomaly, serous retinal detachment is a rare complication that may occur.5 A proposed mechanism for this involves disturbances in the choroid and RPE at the junction of the coloboma and normal tissue, which permit subretinal leakage of fluid. Another rare complication is choroidal neovascularization.2,3 The new vessels are typically noted in the area of disturbed tissue, which may be predisposed to breaks in Bruch’s membrane.
Confirming the diagnosis. Careful clinical examination of the fundus and interpretation of visual fields can confirm the diagnosis of tilted disc syndrome. Intracranial imaging is necessary to rule out chiasmal lesions, especially when the visual field defects respect the midline. Tilted disc syndrome is a benign developmental anatomic variant. Patients typically maintain excellent vision without complications.
Treatment and Outcome
As tilted disc syndrome is a congenital anomaly, and Mrs. Ross had completed intracranial imaging to rule out a chiasmal lesion, no treatment was necessary. Mrs. Ross will continue to be monitored annually for potential hydroxychloroquine toxicity.
Conclusions
Bitemporal visual field defects occur most commonly with chiasmal disorders. Individuals with tilted disc syndrome, a congenital anomaly, may have bitemporal visual field defects that mimic chiasmal disorders. Neuroimaging is essential to rule out intracranial pathology.
___________________________
* Patient name is fictitious.
___________________________
1 Manfrè L et al. Am J Neuroradiol. 1999;20(9):1750-1751.
2 Sowak JW et al. Optometry. 2009;80(5):232-242.
3 Bottoni FG et al. Eye. 1990;4(Pt 3):504-509.
4 Vuori M, Mantyjarvi M. Acta Ophthalmol. 2008;86(6):622-625.
5 Cohen SY et al. Ophthalmology. 1998;105(10):1831-1834.
___________________________
Dr. Schaefer is an oculoplastics fellow at West Virginia University in Morgantown. Dr. Patel is a cornea clinician-scientist and clinical assistant professor of ophthalmology and Dr. Lema is a retina surgeon and clinical assistant professor of ophthalmology; both are at the University of Buffalo’s Ross Eye Institute in Buffalo, New York. Relevant financial disclosures: None.