By Jordan Stanley, MD, and Lanning B. Kline, MD
Edited by Steven J. Gedde, MD
Download PDF
Sam Wilson,* age 54, went to his local emergency room after waking up with decreased vision and pain involving his left eye.
Initial Misdiagnosis
At the first hospital he visited, Mr. Wilson was diagnosed with optic neuritis in his left eye. He was treated with systemic corticosteroids and reported initial improvement in both vision and pain symptoms.
Over the next few months, he saw several ophthalmologists, and there were repeated attempts to taper the steroids, with his vision declining each time. Four months after he was first put on steroids, and after another failed taper, he underwent a vasculitis workup—including a temporal artery biopsy—that was normal.
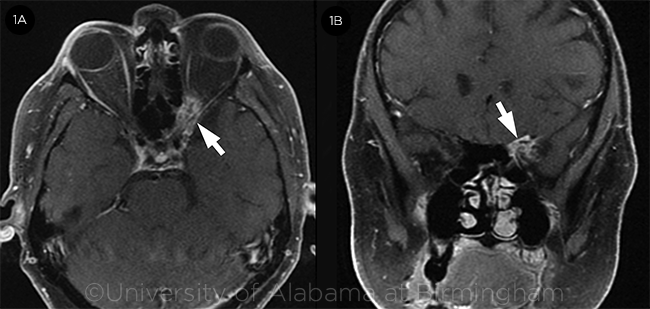
One week later, he experienced an acute decline in vision in his left eye. Orbital magnetic resonance imaging (MRI) demonstrated a small, ill-defined left orbital apex mass measuring 0.9 × 1.5 × 0.9 cm (Fig. 1). It was noted to be abutting, and possibly encasing, the left optic nerve. Mr. Wilson was transferred to our institution.
 |
|
MRI. Postcontrast axial (1A) and coronal (1B) MRI with fat suppression shows enhancement of a left orbital apex lesion (arrows).
|
We Get a Look
We saw Mr. Wilson 5 months after the initial onset of symptoms. His complaints included binocular diplopia and decreased visual acuity, reduced color vision, and pain involving his left eye.
He reported no prior ocular history apart from refractive error.
His medical history included HIV infection (he was adherent to antiretroviral therapy and had a CD4 count of 700 cells/mm3 [normal range: 500-1,500 cells/mm3]), hypertension, hyperlipidemia, and anxiety.
His medications included darunavir, raltegravir, ritonavir, emtricitabine, hydrochlorothiazide, losartan, pravastatin, valaciclovir, alprazolam (as needed), and prednisone.
On exam, he had Cushingoid features from prolonged steroid use. His visual acuity was 20/20 in the right eye and 20/800 in the left. His pupils were equal, round, and reactive, with a left relative afferent pupillary defect. Intraocular pressure was 17 mm Hg in each eye. His right eye had full motility; in his left eye, we noted moderate supraduction, adduction, and infraduction deficits. Ophthalmoscopy revealed a normal right fundus and mild left disc edema without pallor.
Differential Diagnosis
Given Mr. Wilson’s atypical presentation and history consistent with a steroid-responsive orbital lesion, neoplastic processes such as lymphoma or optic nerve sheath meningioma were at the top of our differential. Other possible diagnoses included infections spreading from the sinuses that often involve the orbit. Although bacterial infection or mucormycosis tends to progress quickly, most fungal infections follow a more protracted course. Inflammatory conditions such as sarcoidosis or Tolosa-Hunt syndrome also can cause decreased vision and a painful ophthalmoplegia, as well as demonstrate steroid responsiveness.
 |
|
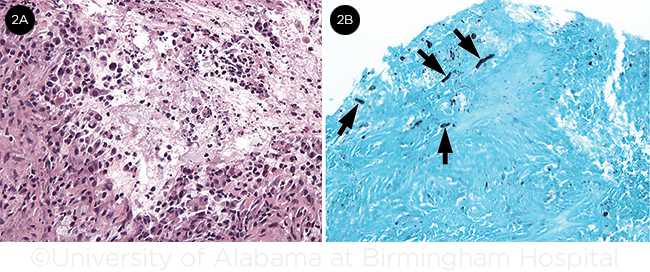
BIOPSY SPECIMEN. (2A) Staining shows evidence of acute and chronic granulomatous inflammation (hematoxylin and eosin, ×20). (2B) Fungal elements (arrows) are present in the specimen (Gomori methenamine silver stain, ×20).
|
Biopsy
The otolaryngology service performed a left orbital apex biopsy via a sphenoid sinus approach and obtained 3 discrete samples: 1 from a mass extending into the sphenoid sinus and the other 2 from the region of the orbital apex. Initial pathology results revealed nonspecific acute and chronic granulomatous inflammation (Fig. 2A). No spindle cells were present, and S100 staining was negative, ruling out meningioma. Flow cytometry was performed but did not demonstrate monoclonal proliferation, ruling out lymphoma.
Acid-fast and fungal stains were performed, and special staining with Gomori methenamine silver stain (GMS) revealed hyphal elements consistent with Aspergillus (Fig. 2B). Culture speciation of A. fumigatus confirmed this.
Discussion
What we saw. Our case demonstrates the difficulty of diagnosing indolent fungal infections involving the orbit. As clinical and imaging findings often can be nonspecific, more common disorders such as idiopathic orbital inflammation and giant cell arteritis (GCA) initially are considered, and treatment for those conditions is started.
A positive response to corticosteroids, as our patient experienced, can give the clinician a false sense of security and further delay diagnosis. The initial perceived benefit of corticosteroids stems from their anti-inflammatory effects. However, their use is ultimately detrimental, as they cause further immunosuppression and allow the pathogens to flourish in the absence of appropriate antifungal therapy. Even though a fulminant invasive course is typical of orbital fungal infection in immunocompromised patients, our patient experienced a slowly progressive course despite his HIV status and chronic steroid treatment.
A wide spectrum of disease. Four main patterns of Aspergillus infection have been characterized.1 Fulminant aspergillosis with vascular and soft tissue infiltration occurs in immunocompromised patients and is often life-threatening, requiring prompt diagnosis and treatment. Treatment includes surgical debridement along with antifungal therapy. While intravenous amphotericin has traditionally been the mainstay, there is growing evidence that voriconazole is an effective and better-tolerated alternative.2
Other patterns often manifest gradually, delaying diagnosis 2 to 10 months after symptoms arise.3 Immunocompromised patients can also experience a chronic invasive infection characterized by granulomatous inflammation, as seen with our patient. In immunocompetent individuals, allergic sinusitis and sinonasal aspergilloma are typical and usually less aggressive.
Recent reports. Hersh et al. reported on a 55-year-old immunocompetent woman with disseminated central nervous system aspergillosis who initially presented with an optic neuropathy, and subsequently experienced stroke in multiple vascular territories.4
While Aspergillus infections have been reported to mimic GCA, the 2 conditions may coexist in rare cases. For example, Zhou et al. described a 75-year-old woman with biopsy-proven GCA with a superimposed orbital apex Aspergillus infection, which resulted in continuing visual decline despite ongoing steroid therapy.5 This case highlights the importance of remaining vigilant for infectious etiologies if the presentation or response to steroids is atypical.
Henderson et al. recently presented a 68-year-old man with invasive aspergillosis that masqueraded as a presumed sphenoid wing meningioma.6 The authors stress the importance of biopsy in cases of presumed meningioma with atypical features.
Take-Away Points
Although aspergillosis may present in a variety of patterns and patient populations, clinicians must maintain a high index of suspicion in the immunocompromised patient when clinical presentations or responses to therapy are atypical. While fulminant fungal infections are often promptly diagnosed, chronic invasive infection is underrecognized, resulting in increased morbidity and even mortality. Neuroimaging and biopsy are paramount in establishing the diagnosis and achieving the best patient outcomes.
Our Patient’s Treatment
Mr. Wilson was started on intravenous amphotericin B, but this was discontinued after 2 days, secondary to rigors. He was then switched to intravenous voriconazole, which was switched to an oral formulation prior to home discharge. The course of oral voriconazole is anticipated to be 6 weeks to 3 months, depending on response.
___________________________
* Patient name is fictitious.
___________________________
1 Levin LA et al. Surv Ophthalmol. 1996;41(2):142-154.
2 Ohlstein DH et al. Case Rep Ophthalmol. 2012;3(1):46-53.
3 Sivak-Callcott JA et al. Br J Ophthalmol. 2004;88(5):681-687.
4 Hersh CM et al. J Neuroophthalmol. 2016;36(4):404-407.
5 Zhou Y et al. J Neuroophthalmol. 2016;36(2):159-163.
6 Henderson AD et al. J Neuroophthalmol. 2017;37(1):105-106.
___________________________
Dr. Stanley is a resident and Dr. Kline is professor of ophthalmology. Both are at the University of Alabama, Birmingham. Financial disclosures: None.