Download PDF
Tear trough deformities can be challenging to treat with dermal fillers, but with proper injection technique and appropriate choice of fillers, physicians can master the rejuvenation of this delicate region. Ophthalmologists do “intricate and precise” every day, and treating patients with tear trough deformities—more accurately known as orbital rim hollows—can be an especially satisfying pursuit for someone with a keen interest in aesthetics.
Three ophthalmologists who have aesthetics-based practices share their insights on the use of hyaluronic acid (HA) fillers to improve tear trough deformities.
Savvy Clientele
Bobby S. Korn, MD, PhD, at UC San Diego Shiley Eye Center, noted that many of his patients are very savvy consumers. “Some want lower eyelid fillers and name the particular filler that they want injected—Belotero, Restylane, or Juvéderm. Other patients want a more permanent treatment and forgo fillers for surgery.” Either way, he and other experts in the field spend much of their time educating patients and managing their expectations.
Initial assessment. Dr. Korn first obtains a detailed history of prior surgery and/or fillers. Next, he examines the lower eyelids, looking for significant fat prolapse, dermatochalasis, and periorbital hollowing, and assessing skin texture and pigmentation.
Clarify patient goals. He then seeks to better understand the patient’s desires and concerns: What is the patient’s goal for lower eyelid rejuvenation? What bothers the patient the most? Dr. Korn gives the patient a handheld mirror and asks him or her to point out specific areas of concern. Then he offers his own suggestions for rejuvenation. Depending on the patient, the best option may be surgery, fillers, or combination treatment. To educate patients, Dr. Korn shows before-and-after photographs of surgeries and filler injections.
Financial considerations. Surgery is more expensive upfront, but the results tend to last longer; fillers are less expensive for a single treatment, require less time to perform, and have less down time, but they require repeat treatment.
Skin quality and tone. Robert A. Goldberg, MD, at UCLA’s Jules Stein Eye Institute, said that patients “come in because they are dissatisfied with how they look, but they don’t necessarily have insight into exactly what age-related changes are causing their discontent.”
He provides patients with a detailed, individualized analysis of age-related factors that play a role in their appearance. Dr. Goldberg maintains that skin quality and skin tone are the most important features in periorbital rejuvenation and are even more important than the orbital rim hollow itself.
“Unfortunately, fillers don’t really address skin quality, although they can help provide some volume and stretching of the skin,” Dr. Goldberg said. “Patients with very thin, inelastic skin usually are not good candidates for fillers. Instead, we try to rejuvenate or rehabilitate the skin because if you use a filler on a patient with poor skin quality, you don’t get the best effect, and the filler actually makes the skin look worse.”
When to refuse. Managing patient expectations is critical. “I certainly have had patients with unrealistic expectations, and I absolutely have turned people away,” said Wendy W. Lee, MD, at Bascom Palmer Eye Institute. “One of the most important tenets in cosmetic medicine is ‘know when to say no’ because so many people who seek cosmetic enhancement have very unrealistic expectations.”
|
Tear Trough Deformity
|
 |
|
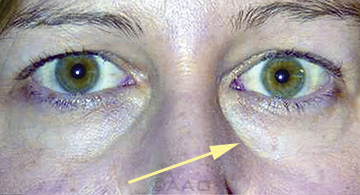
This tear trough deformity is a depression running from the medial canthus along the inferior orbital rim.
|
Filler vs. Surgery
Dr. Lee emphasizes that treatment for tear troughs must be individualized because the structure is different in every patient. “It requires really examining the patient’s anatomy and the degree of her tear trough deformity and being reasonable in what you can achieve with a filler versus surgery,” she said. “Then you can map out whether the patient is a better surgical candidate versus a filler candidate or a candidate for some other modality, such as laser resurfacing. If the patient’s tear troughs are subtle, with just a small contour defect between the eyelid and the cheek, surgery may not be the best option because there may not be enough fat or skin to remove or reposition.”
Some patients simply don’t want to have surgery yet, Dr. Lee added. In these instances, she does less invasive maneuvers like fillers to disguise the appearance of a tear trough or prolapsed fat. Dr. Lee prefers to treat the periocular area with multiple modalities, combining botulinum toxin, dermal fillers, and lasers, along with surgery if necessary. “Each modality treats a specific area—we use botulinum toxin to immobilize the muscles causing the wrinkles, fillers to fill in volume deficits, and the laser to improve skin texture.”
 |
|
FILLER. A 45-year-old woman before (top) and three years after (bottom) hyaluronic acid gel filling of the inferior and superior orbital rim hollow.
|
Contraindications
Adverse reactions to HA fillers are rare, but they can occur. Allergic, anaphylactic, and anaphylactoid reactions have been reported after HA injections. Skin testing for HA fillers is not routinely performed because of the low incidence of allergy compared with earlier products like bovine collagen, which required skin testing.
Patient history is crucial. Getting a good history is important preventive medicine, noted Dr. Korn. Patients with active skin infections in the periocular region should avoid HA filler injections until the condition resolves.
Discuss discoloration. Patients also should be warned that HA injections in the tear troughs can result in a bluish discoloration of the skin, known as the Tyndall effect. Some patients are not bothered by it, whereas others definitely are. Dr. Korn added that some of the newer fillers are less likely to manifest this effect.
Know the fillers. According to Dr. Goldberg, most of the commercial HA fillers share more similarities than differences. “The two products I use around the eye are Belotero and Restylane, but people get good results from all sorts of different fillers,” he said. “However, edema is one of the complications of fillers, and there are some suggestions that Juvéderm may cause a little more edema around the eye. Because the eye is very sensitive to edema, some have argued that Juvéderm, which is a very good filler for several areas of the face, may not be as good for periorbital filling.”
Ten-year results. Dr. Goldberg is currently publishing his group’s 10-year results with fillers. “We have had some patients whose fillers lasted five to seven years. But we found that an average interval for reinjection was more or less one year. As a result, our patients have maintenance injections around the eye every year or two.” He added that it is possible to overfill a patient and that complications tend to arise with too many repeated injections over time. A conservative approach is always better.
Complications
Although the most common complications are lumps, bumps, a blue hue from the Tyndall effect, and hypersensitivity reactions, some complications are more serious.
Swelling. Edema around the eye is a major complication, and it is not entirely clear why it develops. “Some patients are susceptible to it, perhaps because they have preexisting edema, and they may develop a little allergic swelling,” Dr. Goldberg said. “Or they happen to have hypothyroidism or heart disease or some systemic edema, and they tend to get fluid or chronic allergic swelling. These patients can develop even more of a boggy edema that can occur early or late after the injection.”
CRAO. With dermal fillers in general, central retinal artery occlusion (CRAO) is the worst complication because it leads to permanent blindness, Dr. Lee said. Although CRAO is very rare—believed to occur in only 1 in 10,000 injections—anyone who injects filler should keep this potential disaster in mind.
There are many reports of blindness. For example, a recent case series described CRAO resulting from dermal filler injection to the forehead,1 and the Korean Retina Society reported on a retrospective study of 44 patients who developed occlusion of the ophthalmic artery or its branches after cosmetic facial filler injections.2 The authors of the latter study noted that “extreme caution and care should be taken during these injections.”
Dr. Lee said, “Most reported cases involve large boluses given within seconds. Patients experience sharp pain and lose vision immediately. It can happen with any filler, including fat, and in almost any area (glabella, nose, nasolabial folds).” Her recommendations are to inject slowly, don’t use a lot of force, and be aware of the patient’s response. “In the glabellar region (the highest risk area3) stay superficial and away from the neurovascular bundles,” she said.
Dr. Goldberg added that, although cases have been reported from temporal injections, the majority of reports—and the majority of cases that he and his colleagues have managed at UCLA—involved nasal or glabellar injection. “Low pressure injection is likely safer than rapid injection. Slowly moving the needle may be better than injecting a bolus in one area. With fillers that allow reflux, it is appropriate to reflux the syringe (checking for arterial flashback) before injecting,” he said. Cannulas may be less likely to cause intra-arterial injection, but he noted that this is not proven, and blindness has occurred in cases in which a cannula was used.
Other complications. Other risks include tissue necrosis as a result of compression or injecting the filler into a vessel. However, necrosis appears to be more likely to occur with injection in the nose or nasolabial folds than elsewhere on the face.3
Pearls
Dr. Korn shares some of what he has learned in working with hyaluronic acid fillers.
- Use a filler mixed with lidocaine if possible. Most fillers are now formulated with the lidocaine premixed. Physicians can add lidocaine to fillers using a Luer-Lok syringe, but this is considered to be an off-label use.
- Patients with very fair and thin skin may be better candidates for a filler that reduces the Tyndall effect.
- Prior to injection, place a small ice pack on the lower lids. This will provide anesthesia and also induces local vasoconstriction for less bruising.
- To minimize bruising, use a blunt-tipped cannula instead of a needle for injecting the filler. The cannula should be long enough that the entire tear trough region can be filled with a single, remote skin nick incision or as few penetrations of the skin as possible. Dr. Korn prefers a 22-gauge needle for the skin nick and a blunt-tipped 27-gauge cannula for filler injection.
- To minimize intravascular complications, use a retrograde injection technique (injecting product while withdrawing the needle) and slowly deliver the filler in numerous small aliquots.
- When injecting the tear trough region, inject along the inferior orbital rim in a pre-periosteal plane. After each injection pass, gently massage the area to evenly distribute the filler.
- Don’t overinject, as most fillers cause some degree of edema. Check the patient a week later and assess for any areas that need a touch-up.
- Know how to recognize and manage complications. Have a “filler crash cart” on hand with 2 percent nitropaste, fresh hyaluronidase, and warm packs on hand in the event of a vascular occlusive emergency.
|
Postoperative Care
Dr. Korn tells his patients to refrain from strenuous activity for one or two days and to avoid sleeping face down. He also suggests that patients periodically apply ice during the first 24 to 48 hours to minimize the bruising. Dr. Korn usually sees patients the week after he has given a filler injection, and he reassures the patient that it is quite normal to have a minor amount of edema after the filler. If there is any lumpiness in the treated area, he suggests that patients simply use their fingers to massage the area, and it often will smooth out.
___________________________
1 Carle MV et al. JAMA Ophthalmol. 2014;132(5):637-639.
2 Parke KH et al. JAMA Ophthalmol. 2014;132(6):714-723.
3 Tracy L et al. J Plast Reconstr Aesthet Surg. 2014;67(4):564-568.
___________________________
Robert A. Goldberg, MD, is professor and chief of orbital and ophthalmic plastic surgery at UCLA’s Jules Stein Eye Institute. Financial disclosure: Receives grant support from Merz Aesthetics and River Vision.
Bobby S. Korn, MD, PhD, is associate professor of ophthalmology at UC San Diego Shiley Eye Center. Financial disclosure: Receives royalties from Elsevier.
Wendy W. Lee, MD, is associate professor of clinical ophthalmology and dermatology at Bascom Palmer Eye Institute. Financial disclosure: Consults for Allergan Medical, Elizabeth Arden, Lumenis, Medicis Aesthestics, Merz Aesthetics, and Ophthalmology Web.