Using the Double-Layer Sign to Predict Subclinical Macular Neovascularization
By Jean Shaw
Selected By: Andrew P. Schachat, MD
Journal Highlights
Ophthalmology Retina, March 2019
Download PDF
Can the double-layer sign on optical coherence tomography (OCT) images be used to predict the presence of subclinical macular neovascularization (MNV) in cases of dry age-related macular degeneration (AMD)? Shi et al. found that the sign on OCT B-scans was associated with subclinical type 1 MNV and can be used to identify these lesions with good predictive values.
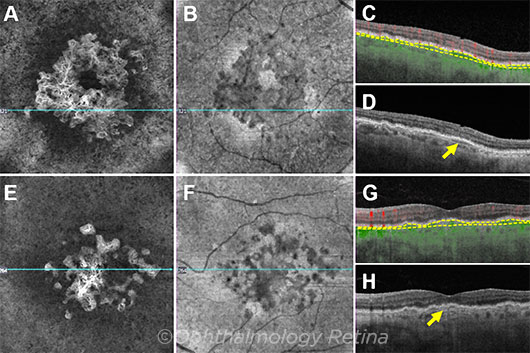 |
AGREEMENT. Graders agreed on the presence of the double-layer sign (yellow arrows) in these two eyes with iAMD and MNV. En face angiographic (A, E) and structural (B, F) images show the CNV pattern. Structural B-scans through the MNV (C, G) are color-coded for flow (red = retinal microvasculature; green = flow under the retinal pigment epithelium [RPE]). The yellow dashed lines represent the slab boundaries from the RPE to Bruch membrane.
|
For this prospective observational study, the researchers evaluated 100 eyes from 94 patients. Of these, 64 eyes had intermediate AMD (iAMD) and 36 eyes had late AMD. Thirty-three eyes had subclinical MNV (20 of the 64 eyes with iAMD and 13 of the 36 eyes with late AMD). All eyes were initially scanned with swept-source OCT angiography (SS-OCTA), using a 6 × 6 mm scan pattern centered on the fovea. All eyes included in the study had no evidence of exudation. Eyes with geographic atrophy (GA) that was not fully contained within the scan area were excluded.
Two groups of graders—including junior graders who had no prior knowledge of the cases—evaluated the B-scans for the presence of the double-layer sign. The senior and junior graders agreed on the presence of a double-layer sign in 24 of the 33 eyes with subclinical MNV and on the absence of the sign in 52 of the 67 eyes without subclinical MNV. For junior graders, the sensitivity, specificity, positive predictive value, and negative predictive value were 73%, 84%, 69%, and 86%, respectively; and for the senior grader, 88%, 87%, 76%, and 94%, respectively. The two gradings also showed that the double-layer sign was a better predictor of subclinical MNV in eyes with drusen than in eyes with GA.
The authors note that the development of a machine-learning algorithm to identify subclinical MNV based on structural OCT is under way. This would be of particular benefit to clinical practices that do not have SS-OCTA capabilities.
The original article can be found here.