By Jeffrey M. Joseph, MD, and Floyd A. Warren, MD
Edited by Thomas A. Oetting, MD
This article is from January 2011 and may contain outdated material.
Ms. Bertha Davis* is well known to our ophthalmology service. She is 64 years old and has a history of hypertension and type 2 diabetes. We saw no pathology at her last yearly exam, but about seven weeks later she began having redness in her right eye, swelling of her right upper eyelid and occasional mild mucus discharge. After 10 days of these symptoms, she went first to her local urgent care center and then to an ophthalmologist close to her home. In both cases, she was diagnosed with conjunctivitis. She was provided with an antibiotic/steroid combination drop and informed that she would improve in the coming days.
But instead of getting better, Ms. Davis felt that the redness was somewhat worse and she experienced “blurry vision” in her right eye. She was not able to characterize this complaint further.
Clinical Presentation
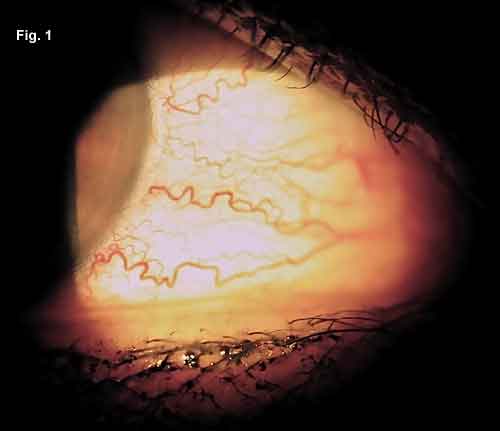
On presentation to our clinic, the patient’s visual acuity was 20/30 in the right eye and 20/25 in the left. Two months earlier, at her annual exam, she had been 20/25 bilaterally. There was no relative afferent pupillary defect. Color vision was normal. Extraocular movements revealed a mild limitation of abduction bilaterally, worse for the right eye. Testing of alignment revealed an 8–prism diopter esotropia at distance and near. The slit-lamp examination was significant for right-sided periorbital edema, with engorgement of the conjunctival vessels (Fig. 1). There were no visible conjunctival follicles or papillae. Normal corneal examinations and deep, quiet anterior chambers bilaterally were noted. IOP was 21 mmHg on the right and 19 mmHg on the left. Exophthalmometry readings were 22 mm on the right and 21 mm on the left with a base of 98 mm. The dilated fundus exam was unremarkable with no optic nerve edema seen.
Upon further questioning after the exam, the patient characterized her complaint of blurry vision as being consistent with, at first, intermittent and, now, constant horizontal binocular diplopia.
Differential Diagnosis
At this point, the clinical presentation represented more than just simple ocular surface inflammation. Given the new-onset diplopia in the setting of a red eye, we suspected an orbital process. And after considering the age, sex and comorbidities of the patient, four categories of causative pathology seemed most likely:
- Inflammatory causes such as thyroid-related orbitopathy or idiopathic orbital inflammation seemed likeliest of all, given the limitation of extraocular movements and the external findings.
- An orbital mass lesion could have been affecting extraocular muscle function and causing vascular congestion, but the lack of proptosis argued against that.
- Vascular causes such as microvascular ischemia needed to be considered, given her history of diabetes and hypertension, but they would not account for her red eye. A vascular malformation could account for the dilated conjunctival vessels, but is not as common as inflammatory causes of new-onset strabismus.
- Last, given the fact that she was diabetic, infection needed to be considered, but this did not seem likely given good, long-standing glycemic control.
Interestingly, the patient had an MRI of the brain performed just three months prior for unexplained headaches. The MRI was felt to be unremarkable by the interpreting radiologist. At this point, we ordered a CT scan of the brain and orbits to better assess the cause of her presentation.
 |
|
AT THE SLIT LAMP. Magnified view of the patient’s right eye demonstrating small, tortuous corkscrew-type blood vessels in the conjunctiva that come up to the limbus and appear different from those seen with other causes of red eye. In contrast to generalized conjunctivitis, these vessels are localized to certain areas, such as the interpalpebral conjunctiva.
|
Diagnosis and Treatment
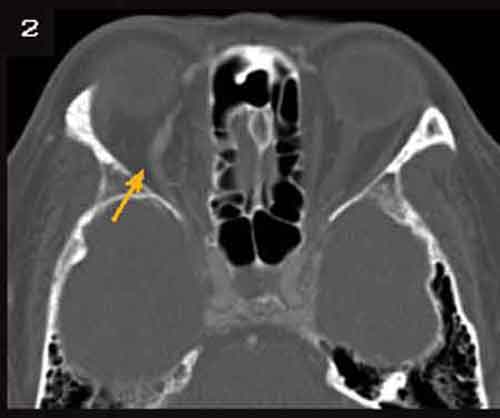
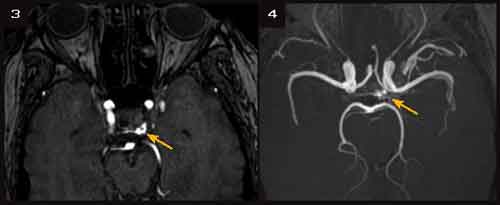
The noncontrast orbital CT showed asymmetric enlargement of the right superior ophthalmic vein and mild right-sided proptosis (Fig. 2). In light of those results, it seemed most likely that a vascular lesion had impaired venous drainage from the orbit. This would account for the dilated conjunctival vessels. The subsequent orbital congestion could account for the motility disturbance. When the patient returned to the clinic, her IOP was asymmetrical (20mmHg on the right, 15 mmHg on the left), with increased pulse pressure on the right. Also, with additional review, she reported an occasional audible bruit, which she described as a “whooshing” noise in her right ear, most prominent when supine. MRI of the brain and orbits and MRA of the head were ordered. The MRI demonstrated small flow voids in the left cavernous sinus in addition to the dilated right superior ophthalmic vein and mild proptosis seen on the CT scan. The MRA demonstrated abnormal signal within the left cavernous sinus and, minimally, in the right posterior cavernous sinus as well (Figs. 3 and 4). There were prominent left sphenoparietal veins extending from the left cavernous sinus.
Combined with the clinical presentation, the imaging led to the diagnosis of low-flow, carotid-cavernous fistula.
After a discussion of the treatment options available, the patient chose conservative management consisting of routine manual carotid compression and close follow-up. She felt that the severity of her symptoms did not warrant the risk of an invasive treatment, such as endovascular embolization.
 |
|
FURTHER IMAGING REVEALS LIKELY CAUSE. On CT, there is dilation of the superior ophthalmic vein and mild right-sided proptosis. The MRA demonstrates the abnormal signal in the left and posterior right cavernous sinus.
|
Discussion
Carotid-cavernous fistula (CCF) is the most common arteriovenous malformation affecting the orbit.1 A CCF is an abnormal communication between the carotid artery and the cavernous sinus. Classification is based on: etiology—traumatic (75 percent) vs. spontaneous (25 percent); velocity of blood flow—high vs. low; and anatomy—direct vs. dural.2 This patient presented with a spontaneous, low-flow fistula that was misdiagnosed as conjunctivitis. Imaging suggested a dural origin, meaning a communication developed between the cavernous sinus and one or more meningeal branches of the internal carotid artery, or the external carotid artery, or both.3
Low-flow fistulas commonly present with subtle signs, as in this case. However, it is important to note that although much less common than in direct fistulas, some visual loss can develop in 20–30 percent of patients. This can be secondary to ischemic optic neuropathy, uncontrolled glaucoma or chorioretinal dysfunction, including central retinal vein occlusion. It is therefore vital to include this in the differential diagnosis of atypical or refractory conjunctivitis, especially in the setting of other findings not typically seen in conjunctivitis.
___________________________
* Patient name is fictitious.
___________________________
Dr. Joseph is chief resident and Dr. Warren is director of neuro-ophthalmology for the department of ophthalmology at both New York University and the Manhattan Eye, Ear and Throat Infirmary.
___________________________
1 Chavish, R. M. et al. “Acute Proptosis in Adults” in Duane’s Clinical Ophthalmology, editors Tasman, W. and E. A. Jaeger. (Philadelphia: J. B. Lippincott, 1994), Vol. 2, Chapter 28, p. 9.
2 Barrow, D. L. et al. J Neurosurg 1985;62:248–256.
3 Das, J. K. et al. Indian J Ophthalmol 2007;55:310–312.