Optical coherence tomography (OCT) is the gold-standard imaging modality for monitoring the posterior segment and a technique that residents will encounter early on in their training.
This article provides a concise summary of how OCT works and also offers some common disease presentations.
How It Works
Spectral-domain OCT (SD-OCT) is the most likely form of OCT that you will encounter in a clinic. SD-OCT provides two- and three-dimensional images with nearcellular resolution (<10 μm). It uses a long-wavelength (near-infrared), broad-bandwidth light source to illuminate the retina and assess the light reflected from retinal tissue interfaces using a spectrometer and Fourier transformation.
This allows for imaging speeds of 40,000 A-scans per second. These rapid imaging speeds can be used to measure the light reflectance from the surface of moving red blood cells. The result is a segmented angiography of the retinal microvasculature, or OCTangiography (OCT-A).
When to Use OCT
The first important clinical decision is when to order an OCT. Although you will use the OCT regularly, it is not advisable for every patient. Asymptomatic patients with excellent visual acuities, for example, may not benefit from imaging.
The highest-yield imaging is performed on symptomatic patients experiencing metamorphopsia, blurred vision or unexplained vision loss. In addition, patients with microvascular disease or structural changes on exam should be imaged. However, OCT should not be used to replace a high-magnification fundus exam.
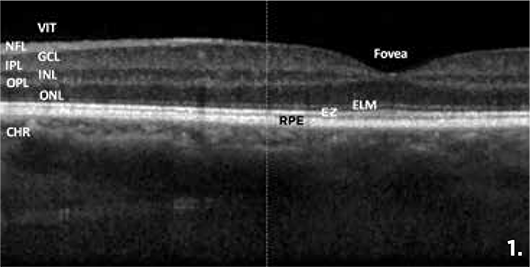
Figure 1 shows an SD-OCT image from a healthy patient. The important layers from the inner to outer retina are: vitreous (VIT), nerve fiber layer (NFL), ganglion cell layer (GCL), inner plexiform layer (IPL), inner nuclear layer (INL), outer plexiform layer (OPL), outer nuclear layer (ONL), external limiting membrane (ELM), inner segment ellipsoid zone (EZ), retinal pigment epithelium (RPE) and choroid (CHR).
To properly evaluate an OCT image, answer these initial structural questions. Is there a normal central macular thickness (CMT) and a normal foveal contour? Is there any retinal thinning or thickening? Is the EZ intact? Is there any outer retinal thinning? Finally, how thick is the choroid?
Common Disease Presentations
Let’s review some clinical images to demonstrate a few important SD-OCT findings.
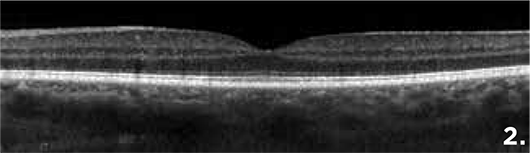
Figure 2 is an image from a healthy patient. Note the foveal contour and CMT (250 μm).
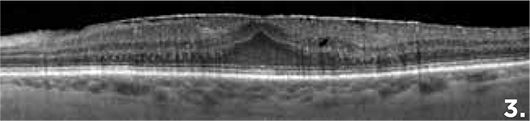
Figure 3 demonstrates an epiretinal membrane on the surface of the retina with a thickened CMT and loss of foveal contour.
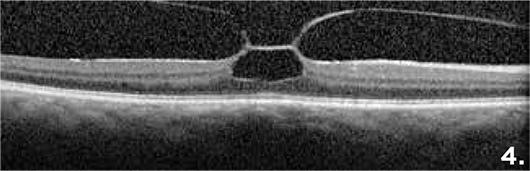
Figure 4 depicts vitreomacular traction with an inverted foveal contour and underlying cavitation.

Figure 5 demonstrates a full-thickness macular hole.
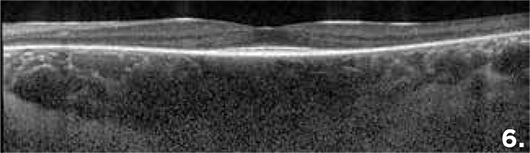
Figure 6 shows severe thinning of the outer retina with sparing of the central EZ. This patient has retinitis pigmentosa.

Figure 7 shows diffuse diabetic macular edema with EZ loss at the fovea.
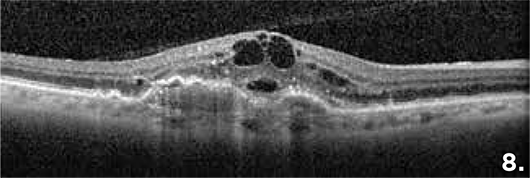
Figure 8 shows a choroidal neovascular membrane in a patient with exudative age-related macular degeneration. Note the fibrovascular pigment epithelial detachment, retinal edema and subretinal fluid.
Hopefully, this concise review will give you a head start in reviewing clinical OCTs. There are many more pearls you will learn in the years to come. Good luck with imaging rounds!
* * *
 About the author:
About the author: Christopher Nathaniel Roybal, MD, PhD, is a retina specialist in private practice at the Eye Associates of New Mexico in Albuquerque and joined the
YO Info Editorial Board in 2017.
![]()