By Sue Vicchrilli, COT, OCS, Academy Director of Coding and Reimbursement, and Jenny Edgar, CPC, CPCO, OCS, Academy Coding Specialist
Download PDF
When physicians hear the word audit, a sense of fear sets in. “Are we documenting correctly? Will we have to pay back money?” The bad news is that post-payment audits frequently uncover discrepancies between what was documented and what was billed, recouping large sums of money for payers. The good news is that you can identify those discrepancies, and correct your future documentation procedures accordingly. Here’s where to start.
Document the History Accurately
The Academy has reviewed more than 800 charts for its members since the recent launch of the Chart-Auditing Service. The most common problems involve incomplete documentation of history.
E&M codes vs. Eye codes. E&M codes have national guidelines for documentation that apply to all physicians. Documentation for Eye codes varies by state and by payer. This article will focus on E&M documentation. (For Eye codes, check the requirements for the payers in your state.)
History has four components. When submitting an E&M code, four components must be documented in the patient’s history: Chief Complaint (CC), History of Present Illness (HPI), Review of Systems (ROS), and Past, Family, and Social History (PFSH). Below, we review the most common mistake made for each of those components.
Chief Complaint
Problem—CC not documented. There needs to be a clear CC indicating the reason for the day’s encounter.
Tip. Ask yourself what is the primary reason the patient came to see you. If there are several reasons, list them in order of importance. While the history does not have to be in the patient’s own words, it may be helpful when capturing something unique to them, such as “I feel like I have crushed potato chips in my eyes.”
The CC is the basis for determining which exam elements are medically necessary to perform.
Why History Matters to Auditors
When you bill for an office visit, there is no one-size-fits-all E&M code that you can use. Instead, you pick from a range of E&M codes—from the established patient’s brief, simple encounter (99211) to the new patient’s complex, time-consuming encounter (99205)—and you are reimbursed accordingly.
Which E&M code applies to a particular office visit? That depends on whether you saw a new patient or an established patient, plus three further criteria:
There are national guidelines that will help you evaluate the facts of a particular office visit so you can determine the relevant history type, exam type, and medical decision-making type. Having determined those criteria, you can consult tables to see which E&M code applies.
Unwritten history. Incomplete documentation of history is a frequent problem. As far as the auditor is concerned, if it isn’t documented then it didn’t happen.
For more on E&M codes—including the tables that indicate which one to use—consider buying The Ophthalmic Coding Series 2015 at www.aao.org/store.
|
History of Present Illness
Common problem—insufficient elements documented. An HPI can be either brief (if it includes one to three of the elements listed below) or extended (four to eight elements). Here are the elements recognized by the guidelines, along with examples of what you might document.
- Location: Left eye, right eye, or both eyes?
- Quality: What is the nature of the problem—constant, acute, chronic, improved, or worsening?
- Severity: How bad is the problem? Describe the pain on a scale of 1 to 10.
- Timing: Is the problem worse in the morning or evening, or is it a constant problem?
- Context: Is it associated with any activity (e.g., blurry while reading)?
- Duration: How long has the patient had this problem—hours, days, weeks, months?
- Associated signs and symptoms: Are there other related problems (e.g., headaches)?
- Modifying factors: What efforts has the patient made to improve the problem (e.g., artificial tears)?
Example. Patient complains of decreased vision OS [Location] for past 4 weeks [Duration] that progressively worsens [Quality] throughout the day [Timing]. Worse when doing near work [Context].
Tip. For an established patient, you can replace the CC and elements of the HPI by documenting the status of three inactive or chronic conditions.
Warning. Don’t clone each record with the same wording, as each encounter should be unique.
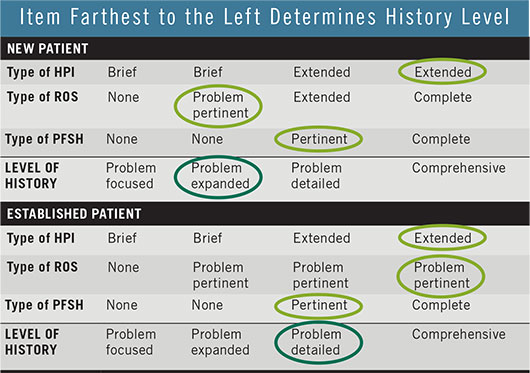 |
The level of history that is involved in an office visit is one of three criteria (along with exam type and complexity of medical decision making) that determine which E&M code can be billed. Find that history level in three steps.
- Determine the type of HPI, ROS, and PFSH.
- Circle the appropriate HPI, ROS, and PFSH, as shown above. Where a row has duplicates (as with HPI’s “Extended”), circle the one to the right.
- The criterion that is farthest to the left determines the level of history.
Example. An exam involves an extended HPI, problem pertinent ROS, and pertinent PFSH. After circling those three elements in the charts above, the most leftward item determines the level of history—in this example, it would be problem expanded for a new patient, problem detailed for an established patient.
|
Review of Systems
Common problem—ROS for new patient is inadequately documented. The ROS may be problem pertinent (only the system in the HPI is reviewed), extended (two to nine systems are reviewed), or complete (10 or more systems are reviewed).
CPT has identified 14 entities or systems that can be part of your ROS. (Click here to download a cheat sheet.)
Tip. Any positives marked on the ROS must be accompanied by a statement of the treatment plan; otherwise, they won’t necessarily count. For instance, if a patient states that she has asthma, you might document that she controls it with an inhaler.
Tip. If the ROS is unobtainable from the patient, state the reason why.
Warning. Be careful not to carry forward your documentation; repeating a comprehensive ROS at every visit can overinflate your level of service.
Past, Family, and Social History
Common problem—PFSH for new patients is missing data. PFSH can comprise three elements:
- Past history, which focuses on prior major illness, operations, current medications, and even allergies.
- Family history should document members of the family who have diseases that may be hereditary, such as glaucoma or diabetes.
- Social history focuses on smoking, drinking, and drug use, as well as employment or job duties.
Tip. While you might not need to report all three elements for established patients, new patients require all three for a complete PFSH.
Take Preventive Action
Update your forms. Review your medical history sheets and make any necessary changes to ensure you have enough room to document both ROS and PFSH appropriately. For examples of medical history sheets, visit www. aao.org/forms.
Review your charts. The Academy can review a sample of your charts to identify any areas of vulnerability (visit www.aao.org/audit for pricing and a summary of how the Chart-Auditing Service works).