Download PDF
One morning, Mark Mario* woke up with a tender, swollen left eyelid. The 8-year-old had a history of sinus infections but otherwise had been in good health, with no history of trauma or recent illness. After several days of worsening swelling and pain, Mark’s mother sought help.
At the pediatrician’s office. When Mark presented at the pediatrician’s office, he was afebrile and, overall, seemed well—except for his left eyelid, which was swollen, droopy, and painful. The pediatrician found the left eyelid tender to touch and was concerned that he might have early preseptal cellulitis, so she prescribed a 2-week course of Augmentin (amoxicillin with clavulanate). When Mark’s condition did not improve after 1 week, she referred him to us.
What We Saw
On examination, Mark’s best-corrected visual acuity was 20/20 in the right eye and 20/25 in the left. There was no afferent pupillary defect in either eye, and his color vision was full. His intraocular pressure was 16 mm Hg in the right eye and 13 mm Hg in the left.
Most remarkable was the fullness of his left eyelid (Fig. 1). On palpation, he had a firm, nonmobile, approximately 2-cm mass of the left anterior orbit. It was contiguous with the left superior orbital rim and was tender to light touch. The mass limited his eyelid elevation, and he demonstrated ptosis with an associated superior visual field defect to confrontation.
Eyelid eversion was difficult due to pain and mass effect; however, the palpebral conjunctiva appeared normal. Mark had mild hypoglobus but no axial proptosis. He had symmetric sensation in the V1-V3 distribution on both sides. His slit-lamp exam was normal in both eyes, and he had a normal fundus exam without evidence of retrobulbar mass effect.
 |
|
WHEN WE FIRST SAW MARK. His left eyelid was swollen, and we noted trace ptosis and hypoglobus.
|
Our Differential Diagnosis
It was apparent to us that this lesion was not a preseptal or orbital cellulitis, as even an abscess would not cause such a very firm lesion in the anterior orbit, and Mark seemed too well overall to have an aggressive orbital infection.
A rapidly appearing orbital lesion in a child always gives the ophthalmologist a sense of fear, with rhabdomyosarcoma, metastatic neuroblastoma, osteosarcoma, and leukemia jumping quickly to mind. However, we didn’t see the proptosis typical of rhabdomyosarcoma, nor the typical ecchymoses of orbital neuroblastoma. Lymphangioma seemed possible given the rapid onset, but there was no antecedent upper respiratory infection. An eosinophilic granuloma seemed possible especially given the bony pain, although it is less common in children than the previously mentioned orbital neoplasms.
We Send Mark to the ED
With a high level of concern, we immediately sent our patient to the emergency department for radiologic studies and a systemic investigation for a potential malignancy.
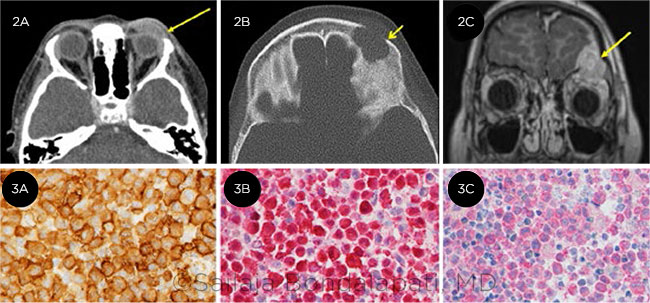
A computed tomography (CT) scan showed an enhancing soft-tissue mass centered in the left frontal bone and left orbital roof with erosion into the frontal bone (Figs. 2A and 2B). Same-day magnetic resonance imaging (MRI) demonstrated a mass effect on the dura and left frontal lobe (Fig. 2C). A thorough systemic lab workup was unremarkable except for an elevated eosinophil count.
Otolaryngology performed an image-guided biopsy of the lesion through a left medial supraorbital incision; a soft-tissue mass that appeared granulomatous was noted intraoperatively.
Frozen tissue analysis revealed multiple eosinophilic granules and dendritic cells positive for the CD1a and S100 markers and the BRAF V600E mutation (Fig. 3), confirming that Mark had Langerhans cell histiocytosis (LCH), formerly known as histiocytosis x.
 |
|
IMAGING AND SOFT TISSUE ANALYSIS. CT scan shows (2A,B) soft tissue mass. MRI (2C) demonstrates erosion of the orbital roof. There was positive staining for (3A) CD1a, (3B) S100, and (3C) BRAF mutation.
|
Discussion
LCH is a rare medical condition of unclear etiology that commonly presents with a triad of exophthalmos, diabetes insipidus, and solitary bone lesions (eosinophilic granuloma). Other variants reported in the literature are Hand-Schüller-Christian disease and, if infants present with severely disseminated disease, Letterer-Siwe disease.
In 1893, Alfred Hand initially misdiagnosed a young child with polyuria, exophthalmos, and skull lesions as tuberculosis.1 Later—in collaboration with Artur Schüller and Henry Christian—Hand coined the term histiocytosis for this medical condition, which has characteristics of multiple skeletal lesions, pituitary infiltration, and exophthalmos.
Incidence. In the United States, the incidence is rare (5-6 cases per million per year); most patients are between 5 and 15 years old. The incidence in males is 2 to 3 times greater than in females.2
Presentation. Patients usually see a pediatrician or an orthopedist for bone pain before the diagnosis is made. Disease presentation is variable, with bone being the most commonly affected organ in up to 80% of cases.2 Skin is the next most frequent site of involvement, followed by pituitary, liver, spleen, lungs, and lymph nodes.
Neuroendocrinopathies related to hormonal deficiencies (such as polyuria from diabetes insipidus, growth failure, and gonadotropin disturbances) are also reported due to both anterior and posterior pituitary involvement.3
Evaluation and diagnosis. A thorough physical exam is essential. This should include inspection of skin and mucous membranes. Laboratory studies should include a complete blood count and basic chemistry, urinalysis, inflammatory markers, thyroid, and coagulation studies. Radiological studies delineate bone and tissue involvement, and histopathological analysis is required for confirmative diagnosis.
Treatment. Multiple treatment modalities are reported in the literature, including observation, surgical resection, localized high-dose steroids, radiation, and chemotherapy, which are tailored depending on the organ involvement and medical conditions of the patient.4 The multitude of treatments reflects the spectrum of disease presentations—although the treatment of choice for isolated lesions is usually excision or local radiation therapy to limit systemic morbidity.
Prognosis. The prognosis is excellent, with 1 study reporting a 10-year survival rate of 100%, with low rates of recurrence for monostotic disease and 71% recurrence for multiorgan disease.5
Mark’s Treatment
Following the orbital biopsy, a full-body positron emission tomography (PET) scan was performed to search for other sites of involvement. This was negative, and our neurosurgery colleagues recommended surgical excision and reconstruction to decompress his orbit and reconstruct the orbital bar and roof.
Two weeks following Mark’s initial presentation to the ophthalmology clinic, he underwent left eyebrow craniotomy with resection of the tumor. The surgery was successful at eliminating the mass effect, and his pain, ptosis, and extraocular motility restriction have resolved (Fig. 4).
Mark continues to demonstrate a postsurgical hypoesthesia in the left V1 distribution as well as a left frontalis palsy. Every 4 months, he is checked by the oncology service to assess for local recurrence, with skull plain films, and he undergoes urinalysis to rule out diabetes insipidus.
 |
|
AFTER SURGERY. Improvement at 3-month follow-up visit.
|
Conclusion
LCH is a rare neoplasm in children but should be considered in patients who present with orbital lesions, especially if they are experiencing bone pain.
Bony erosion on imaging is a hallmark of the disease, although it may be seen in other orbital lesions, both malignant and benign.
Surgical biopsy is needed for definitive diagnosis; once confirmed, a finding of eosinophilic granuloma should prompt complete systemic evaluation for other sites of disease.
___________________________
* Patient name is fictitious.
___________________________
1 Badalian-Very G et al. Annu Rev Pathol. 2013;8:1-20.
2 Khatami et al. Pakistan Journal Radiology. 2010;20(3):114-120.
3 Haupt R et al. Pediatr Blood Cancer. 2013;60(2):175-184.
4 DiCaprio MR et al. J Am Acad Orthop Surg. 2014;22(10):643-652.
5 Maria Postini A et al. J Pediatr Hematol Oncol. 2012;34(5):353-358.
___________________________
Dr. Cohen is a comprehensive ophthalmologist, Dr. Grace is a pediatric ophthalmologist, and Dr. Bondalapati is an ophthalmology resident; all 3 are at The Kittner Eye Center at The University of North Carolina Hospitals in Chapel Hill, N.C. Financial disclosures: None.