By Michael Paap, BA, and Rona Z. Silkiss, MD, FACS
Edited By: Steven J. Gedde, MD
Download PDF
Laura Lee* was growing increasingly concerned. Several months earlier, the 47-year-old had noticed an area of fullness in her right upper eyelid (Fig. 1). Although she didn’t think much of it at the time, she began to feel uneasy as the mass grew and became readily visible. When it started feeling tender to the touch, she decided to make an appointment with her local ophthalmologist. He subsequently referred her to our clinic.
We Get a Look
History. During her visit to our oculoplastics clinic, Ms. Lee reported no significant medical history or recent ocular trauma. She also denied a history of past eyelid lesions, diplopia, visual changes, or eye surgery. She was worried that the growing mass was indicative of cancer. Given the lesion’s tenderness and relatively rapid growth, we were similarly concerned about the possibility of an orbital neoplasm.
Exam. On initial exam, we confirmed a mass in the right upper lid in the area of the lacrimal gland as well as mild right proptosis. The remainder of her external and anterior segment ophthalmic exam was within normal limits.
 |
|
PRESENTATION. Preoperative appearance of patient showing swelling of the right upper eyelid.
|
Testing
Imaging. Following her appointment, we ordered magnetic resonance imaging (MRI), which showed a well-circumscribed, heterogeneously enhancing mass in the extraconal space of the right upper quadrant. It measured 30 × 16 × 21 mm and had at least one 5-mm cyst within its borders. Although the features of this mass were consistent with pleomorphic adenoma (PA), they were not specific enough to exclude other types of lacrimal gland neoplasms, possibly malignant.
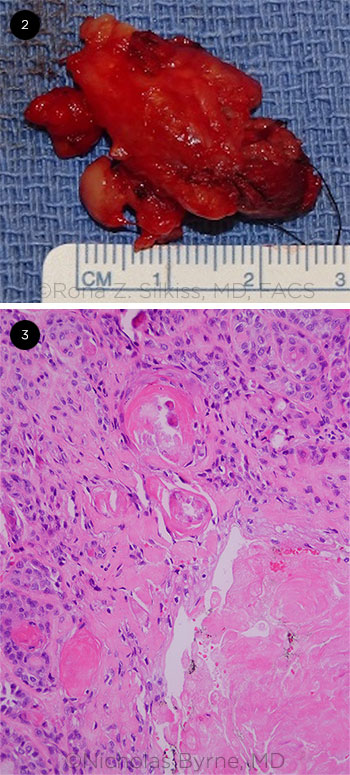
Mass removal. We excised the lesion using a right lateral orbitotomy approach under laryngeal mask anesthesia and preserved it for examination (Fig. 2). Ms. Lee tolerated the procedure well and, within two weeks, reported no residual pain or swelling.
Pathology report. Microscopic evaluation demonstrated a mitotically active basaloid epithelial neoplasm lining an expanded lacrimal duct with multiple squamous eddies. Reduplication of basement membrane–like material within and around the periphery of the tumor provided further evidence to support a diagnosis of PA, also known as benign mixed tumor (Fig. 3). However, the increased rate of mitosis, in addition to the interspersed central areas of fibrosis and necrosis, made us concerned about aggressive behavior. The pathology results were inconclusive, and other options on our broad differential diagnosis included basal cell neoplasm, myoepithelial neoplasm, carcinoma ex pleomorphic adenoma, and aggressive salivary neoplasm not otherwise specified. Salivary tumor was included in the differential because of the histologic similarity between salivary and lacrimal gland tumors as well as previously documented cases of spontaneous emergence of salivary tumors in the orbital region.1
To better characterize the lesion, pathology then performed a panel of immunohistochemical stains. A positive staining pattern for SOX10, S100, CK5/6, and p63 generally supported the morphologic impression of a lacrimal salivary gland tumor. A fluorescence in situ hybridization study with the EWSR1 separation probe was negative for the separation of 5´ and 3´ EWSR1 signals, providing no further support for a diagnosis of myoepithelial neoplasm. The combined histologic, immunostaining, and cytogenetic pattern were most supportive of a benign mixed tumor with aggressive features.
 |
|
EX VIVO. (2) Tumor following surgical excision. (3) Overview of tumor histology, showing regions of increased mitotic activity, abnormal matrix production, squamatization, and calcification. H&E stain, 200× magnification.
|
Discussion
Lacrimal gland masses can broadly be classified as inflammatory lesions, epithelial tumors, metastatic cancer, and lymphomas. Diagnosing epithelial lacrimal tumors can present a challenge, even with histologic evaluation, because of the morphalogic diversity within each subtype of this group.
Pleomorphic adenomas. PAs are the most common type of epithelial tumor, comprising 41% of cases.2 Although they are classically characterized microscopically by heterogeneous inclusion of epithelial, myoepithelial, and mesenchymal tissue, PAs exhibit significant variation in the appearance and proportion of their cell components.3 Diagnosis of PA is further complicated by the possibility of malignant transformation, which occurs in 10% to 20% of cases, most frequently developing into a pleomorphic adenocarcinoma.4 Although features such as necrosis and increased mitosis are suggestive of malignancy, they are not definitive, and classification of this type of tumor may be difficult.4
Differentiation. Despite these challenges, it’s important to differentiate between benign and malignant lacrimal tumors given their drastically different prognoses. Immunohistochemistry can be a helpful tool, as many different tumors exhibit association with specific stains. For example, myoepithelial carcinomas are associated with CK5/6, p63, and S100.5 However, as in this case, staining patterns can indicate more than one possibility such as mixed tumor. The value of imaging studies is also limited; although a lesion that appears well circumscribed on MRI or computed tomography is typically benign, an early-stage malignancy may have a similar appearance.6
Several general clinical features are also suggestive of lacrimal neoplasm malignancy, including rapid onset of symptoms and presence of pain,7 both of which were present in Ms. Lee. However, benign lacrimal tumors such as PAs have also been histologically diagnosed in cases in which features such as pain, rapid progression, and orbital bone destruction might otherwise suggest a malignancy.8
Conclusion
This case presents a challenging and inconclusive diagnosis of a lacrimal gland tumor. Based on current histopathologic, radiographic, immunohistochemical, and clinical evaluation, we are unable to definitively classify it beyond mixed tumor with aggressive features. Given the uncertainties inherent in managing poorly defined tumors, we believe this case underscores the need for conservative treatment and frequent follow-up.
Our Patient
Ms. Lee healed well following excision of the mass. Because of the possibility of recurrence and residual malignancy, we referred her for an evaluation for postoperative radiation therapy. This treatment was declined by the patient. She will be monitored with regular MRI imaging and follow-up for any evidence of recurrence.
___________________________
* Patient name is fictitious.
___________________________
1 Kuo YL et al. Eur Arch Otorhinolaryngol. 2011;268(7):1035-1040.
2 Font RL et al. Arch Ophthalmol. 1998;116(5):613-616.
3 Harrison W et al. Saudi J Ophthalmol. 2018;32(1):13-16.
4 Rose GE, Wright JE. Br J Ophthalmol. 1992;76(7):395-400.
5 Argyris PP et al. Head Neck Pathol. 2013;7(1):85-92.
6 Shields CL, Shields JA. Int Ophthalmol Clin. 1993;33(3):181-188.
7 Perzin KH et al. Cancer. 1980;45(10):2593-2606.
8 Miyazaki T et al. Neurol Med Chir (Tokyo). 2005;45(8):407-410.
___________________________
Mr. Paap is a second-year medical student at the University of California, San Diego, in La Jolla, Calif. Dr. Silkiss is Chief of Oculofacial Plastic Surgery at California Pacific Medical Center in San Francisco. Relevant financial disclosures: None.
Write a Morning Rounds Article
Share an intriguing case report with your colleagues. Here’s how:
1) Introduce the patient (fictitious names only) and describe his or her personal story and baffling symptoms.
2) Then move on to any of the following areas: early misdiagnoses, your observations, differential diagnosis, results of tests, the eventual definitive diagnosis, treatment, and the patient’s progress.
3) Add a few short paragraphs about the disease to augment readers’ knowledge base (pathophysiology, etiology, etc).
To get started, visit aao.org/eyenet/write-for-us.
Are you a resident? A resident article published in the Morning Rounds section will satisfy the RRC requirements for resident scholarly activity.
|