By Lori Baker-Schena, MBA, EdD, Contributing Writer, interviewing Ahmad A. Aref, MD, Seenu M. Hariprasad, MD, Mathew W. Maccumber, MD, PhD, and Jeremy B. Wingard, MD
Download PDF
The question appears straightforward enough: Do repeated intravitreal anti–vascular endothelial growth factor (VEGF) injections cause a long-term increase in glaucoma or ocular hypertension (OHT) in patients with neovascular age-related macular degeneration (AMD)?
A review of the literature indicates the answer is not that simple.
While earlier studies showed a minimal risk of sustained elevated intraocular pressure (IOP) following intravitreal anti-VEGF injection, a more recent retrospective clinical study demonstrated a significantly increased incidence of OHT and open-angle glaucoma (OAG) related to this treatment.1
One thing is for certain, according to Ahmad A. Aref, MD, at the University of Illinois Eye and Ear Infirmary in Chicago. “Given the severity of AMD and glaucoma, both of which can lead to irreversible blindness, and the increasing numbers of older patients who will need anti-VEGF intravitreal injection therapy, sustained IOP elevation following anti-VEGF injections will continue to be an important area of research.”
Pathophysiology Still Being Explored
Dr. Aref explained that 2 distinguishable time periods of IOP elevation following intravitreal anti-VEGF injections—short-term and long-term—have been identified.2
Short term. Short-term increases in IOP are seen almost immediately following injection, and from a pathophysiology perspective they are thought to be related directly to an increase in intraocular fluid volume. “Typically, the rise is by virtue of injecting fluid into a restricted space,” he said.
Long term. On the other hand, the pathogenesis of long-term, sustained IOP elevation has been more difficult to ascertain, Dr. Aref said. “Theories include a permanent decrease in outflow facility due to repeated spikes in IOP after each injection that damage the trabecular meshwork; direct pharmacological toxicity; and chronic trabeculitis.”
He pointed to a recent study showing that chronic anti-VEGF injections significantly reduced outflow facility in patients with AMD.3 Researchers found a small but statistically significant decrease in tonographic outflow facility in patients who had undergone 20 or more anti-VEGF injections; this decrease was not observed in patients with 10 or fewer injections. The researchers also showed that patients with ocular hypertension in their uninjected eye demonstrated a substantially lower outflow facility in their injected eye.
“The pathogenesis of sustained IOP increases associated with anti-VEGF remains unclear and continues to be the focus of many studies,” he said.
 |
|
INJECTION. It is generally agreed that the fluid introduced by intravitreal anti-VEGF injection raises IOP over the short term. However, expert opinion differs about the long-term effects of these injections.
|
A Minimal Concern
Researchers appear to agree that short-term IOP increases after anti-VEGF injections frequently occur. Seenu M. Hariprasad, MD, at the University of Chicago, noted that several papers over the years have described this phenomenon.
“In each of these studies, a significant elevation in IOP was found 30 minutes after the injection but returned to baseline levels by the first follow-up clinic visit,” Dr. Hariprasad said. “My own research looking at pegaptanib, bevacizumab, and ranibizumab also indicated that the IOP increase we saw roughly 30 minutes after the injection had normalized at the 5- to 7-day follow-up visit.”4-6
While the short-term IOP rise is almost universally understood and accepted, Dr. Hariprasad said, the debate surrounding whether these injections cause long-term elevation in IOP persists. He added that several large clinical trials have demonstrated that intravitreal injections “very rarely” led to a sustained increase in IOP.
This includes the post hoc analysis of the Minimally Classic/Occult Trial of the Anti-VEGF Antibody Ranibizumab in the Treatment of Neovascular AMD (MARINA) and the Anti-VEGF Antibody for the Treatment of Predominantly Classic Choroidal Neovascularization in AMD (ANCHOR) ranibizumab trials,7 “which showed that most ranibizumab-treated eyes did not experience a sustained elevation of IOP over 24 months,” he said.
New study. “Yet despite these findings, a recent survey of retina specialists revealed that 55% believe intravitreal injections may cause sustained IOP elevation,”8 Dr. Hariprasad said. “Realizing the need for further clarification, we recently published a retrospective study investigating how the number and timing of intravitreal injections in patients with AMD and DME [diabetic macular edema] affected IOP over time.”9
Long-term IOP data were collected on 76 AMD patients and 55 DME patients receiving anti-VEGF injections at Dr. Hariprasad’s institution. Time points ranged from 0 to more than 24 months, with patients receiving from 1 to more than 10 injections. “Our data suggested that when using a treat-and-extend dosing regimen, the administration of anti-VEGF intravitreal injections was not a significant risk factor for an increase in IOP—regardless of how many injections the patient received,” he said.
Conclusion. Dr. Hariprasad said that after looking at the evidence from these studies, “the argument is very weak that anti-VEGF injections cause a meaningful long-term increase in IOP.” And, although clinical judgment is advised for patients at risk for glaucoma, “clinicians should use anti-VEGF agents with confidence that long-term IOP elevations are of minimal concern,” he said.
An Important Link
Jeremy B. Wingard, MD, at the Wheaton Eye Clinic in Illinois, was prompted to conduct a controlled retrospective chart review1 after observing a significant incidence of sustained OHT and OAG in AMD patients receiving anti-VEGF intravitreal injections.
Trends in the clinic. “Wheaton Eye Clinic is one of the largest practices in the Midwest with more than 30 ophthalmologists, including 5 retina specialists and 5 glaucoma specialists,” he said. “Our size and internal referral system allow us to study disease development in a highly controlled manner and with numbers that vastly exceed other studies looking at individual patient results. Our retina specialists were directly referring their AMD patients to our glaucoma specialists for sustained ocular hypertension, and we wanted to further study this phenomenon.”
The study. Dr. Wingard noted that the retrospective chart review only included patients who received unilateral anti-VEGF injections but in whom both eyes could be analyzed to determine OHT or OAG development. Of the 1,107 patients who met the study criteria, 43 (3.88%) developed OHT or OAG in only the injected eye, 21 patients (1.90%) developed OHT or OAG in both eyes, and 2 patients (0.18%) developed OHT or OAG only in the untreated eye.
“The most striking finding is that 30 patients received 25 or more injectionsof bevacizumab, and of those 30 patients, 11, or 36.7%, developed OHT or OAG in the treated eye only,” Dr. Wingard noted. “A number of these patients needed surgery to manage their glaucoma. In fact, of the 40 patients who developed glaucoma in the treated eye and were followed by our glaucoma specialists for at least 6 months, 35% required glaucoma surgery to manage their disease, including 17.5% who required filtering surgery. Thankfully, these surgical patients have generally responded well to treatment and have been able to resume anti-VEGF injections as indicated for their AMD.”
Dr. Wingard noted that some earlier, and typically small, studies did not identify this link as they rarely included patients who had more than 25 injections, and yet this population is crucial given the chronic nature of AMD. “You can’t stop delivering the anti-VEGF medication in many of these patients,” he said. “Most retina doctors are trying to extend the time between the injections, but in certain patients, there is a risk to this strategy as well. And the longer patients live, the more injections they will need.”
Conclusion. “It is important to bring this information to light as it supports the hypothesis that intravitreal anti-VEGF injections have a significantimpact on sustained IOP elevations,” he added. “I am personally convinced that there is a cause and effect, and any new anti-VEGF regimens that are tested should prospectively assess patients for the possible development of sustained ocular hypertension and optic nerve damage.”
IOP Rise Uncommon
The 2013 introduction of the Academy IRIS Registry (Intelligent Research in Sight), which includes clinical benchmarks and practice patterns on more than 28 million U.S. patients and 100 million patient visits, has given practicing ophthalmologists new insights through big data, noted Mathew W. MacCumber, MD, PhD, at Rush University Medical Center in Chicago.
“Several previous studies have suggested a link between intravitreal anti-VEGF injections and sustained IOP,” noted Dr. MacCumber. “We wanted to use the power of real-world big data to gain clarification.”
The study. At the 2017 ARVO meeting in May, Dr. MacCumber and colleagues presented study findings indicating that overall anti-VEGF therapy was in fact associated with a small decrease in IOP over time.10
The study included 23,282 patients in the IRIS Registry with AMD, DME, or branch or central retinal vein occlusion who received bevacizumab, ranibizumab, or aflibercept injections in the right eye from the study period between Jan. 1, 2013, and Dec. 31, 2015.
“When looking at the 3 drugs, IOP was generally higher in bevacizumab-treated eyes compared to aflibercept- and ranibizumab-treated eyes, although the differences were small. Moreover, when looking at the rate of a clinically significant pressure rise [at least a 6 mm Hg IOP rise to over 21 mm Hg], the rate was 2.2% for aflibercept, 2.5% for ranibizumab, and 3% for bevacizumab,” Dr. MacCumber said.
Dr. MacCumber noted the IRIS Registry findings supported Dr. Wingard’s clinical results to some extent and extended them further for a comparison between the 3 commonly used anti-VEGF drugs. “When we ran numbers on the IRIS Registry data for the 324 patients who had 25 or more injections, we saw that bevacizumab caused more eyes to develop high IOP, 4%-9.5%, not as high as his study at 36%,” Dr. MacCumber added. “The other 2 drugs still caused only 1%-3% of injected eyes to experience a clinically significant pressure rise.”
Dr. MacCumber noted that the overall lower rates of sustained IOP found in the IRIS Registry data reflected practice patterns from thousands of ophthalmology practices, unlike the smaller populations seen in clinical trials, which may explain his study’s findings.
Conclusion. “While we agree that there are eye pressure rises associated with anti-VEGF injections, it is generally less common than previously reported,” said Dr. MacCumber.
More at the Meeting
Subspecialty Day takes place Friday, Nov. 10, and Saturday Nov. 11, in New Orleans. While the glaucoma program is a Saturday-only event, the retina program spans both days. In addition to presentations delivered by experts on timely topics, the program includes lively discussion about issues of clinical interest, including:
- Circadian Factors in Glaucoma Progression, Daytime/Nighttime
- OCT Angiography Is Ready for Mainstream Clinical Use, Pro/Con (retina)
For the most current 2017 Subspecialty Day program schedules, choose your area of interest at aao.org/annual-meeting/subspecialty-day.
|
Implications for Practice
While questions of elevated IOP after anti-VEGF injections continue to be explored, clinicians can take steps now to protect their patients, noted Dr. Aref.
“First, if clinicians are considering starting a patient on anti-VEGF treatment, they should obtain accurate measurements of baseline eye pressures and optic nerve status, as well as determine the patient’s risk for glaucoma. If the patient is diagnosed with glaucoma or deemed to be at a substantially increased risk, he or she should be treated accordingly before undergoing the injections.”
Second, if the patient is at an average risk for glaucoma, the clinician should do “whatever it takes” to treat the macular degeneration. “Keep monitoring the IOP,” Dr. Aref added, “and if an IOP increase continues to appear sustained over several months, a different treatment strategy should be considered.” This may include changing anti-VEGF medications or switching to a treat-and-extend strategy.
Finally, Dr. Aref stressed that retina specialists should develop strong working relationships with their glaucoma colleagues. “It’s important to get these complicated patients evaluated to determine the optimal treatment.”
___________________________
1 Houlihan N, Lin J, Gieser J, Delzell D, Wingard J. Poster #135, The relationship between anti-VEGF treatments and the development of glaucoma or ocular hypertension in macular degeneration patients. Presented at: American Glaucoma Society 2017 Annual Meeting; May 4, 2017, Coronado, Calif.
2 Aref AA. Curr Opin Ophthalmol. 2012;23(2):105-110.
3 Wen JC, Reina-Torres E, Sherwood JM, Challa P, Liu KC, Li G, Chang JYH, Cousins SW, Schuman SG, Mettu PS, Stamer WD, Overby DR, Allingham RR. Invest Ophthalmol Vis Sci. 2017;58(3):1893-1898.
4 Hariprasad SM, Shah GK, Binder KJ. Am J Ophthalmol. 2006;141(1):200-201.
5 Mazzulla DA, Hariprasad SM, Jager RD, Mieler WF. Retin Cases Brief Rep. 2008;2(3):234-235.
6 Mojica G, Hariprasad SM, Jager RD, Mieler WF. Br J Ophthalmol. 2008;92(4):584.
7 Bakri SJ, Moshfeghi DM, Francom S, Rundle AC, Reshef DS, Lee PP, Schaeffer C, Rubio RG, Lai P. Ophthalmology. 2014;121(5):1102-1108.
8 Yannuzzi NA, Patel SN, Bhavsar KV, Sugiguchi F, Freund KB. Am J Ophthalmol. 2014;158(2):319-327.e2.
9 Nariani A, Williams B, Hariprasad SM. Indian J Ophthalmol. 2016;64(9):643-647.
10 Atchison EA, Barry CN, Lum F, Mattox C, MacCumber MW. Poster # A0050, The real world effect of anti-VEGF injections on IOP using the IRIS Registry. Presented at: ARVO Annual Meeting; May 7, 2017, Baltimore.
___________________________
Dr. Aref is assistant professor of ophthalmology, Glaucoma Service, and director, Residency Training Program, Illinois Eye and Ear Infirmary, University of Illinois College of Medicine, Chicago. Relevant financial disclosures: None
Dr. Hariprasad is Shui-Chin Lee Professor of Ophthalmology and Visual Science, chief, Vitreoretinal Service and director, Clinical Research at the University of Chicago Medicine & Biological Sciences. Relevant financial disclosures: Regeneron: C,L.
Dr. MacCumber is professor and associate chairman for research, Department of Ophthalmology, Rush University Medical Center, Chicago. Relevant financial disclosures: Genentech: C,S; Regeneron: C,S.
Dr. Wingard specializes in glaucoma and cataract surgery at Wheaton Eye Clinic, Wheaton, Ill. Relevant financial disclosures: None.
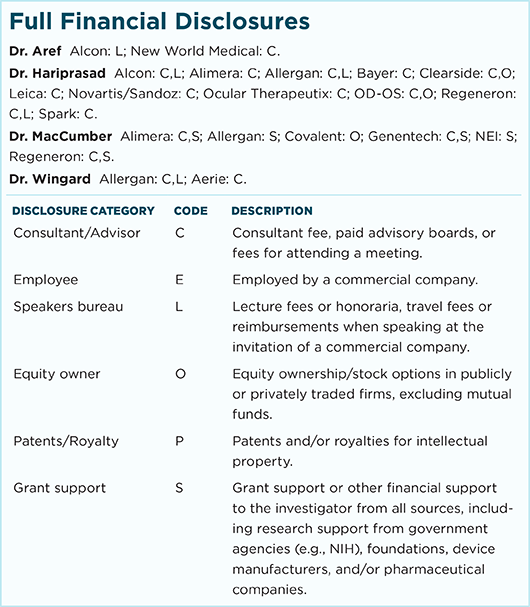
For full disclosures and the disclosure key, see below.