Blink
MAR 01, 2019
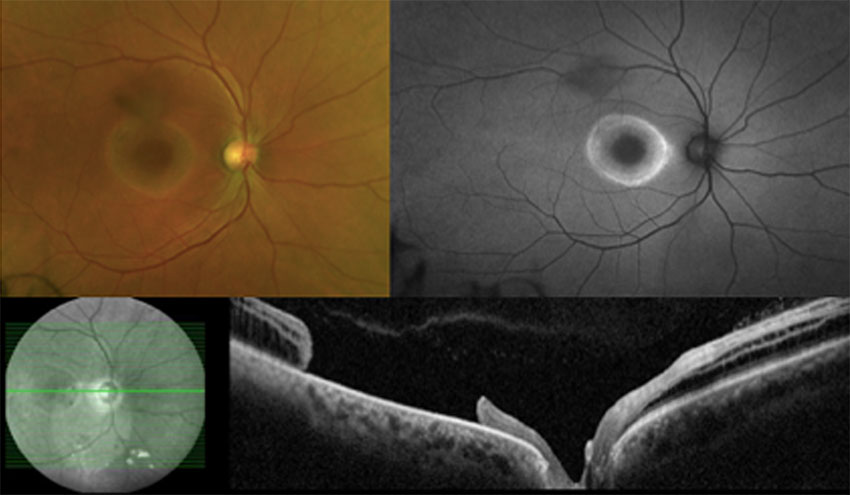
Can You Guess March's Mystery Condition?
Download PDF
Make your diagnosis in the comments, and look for the answer in next month’s Blink.
Last Month’s Blink
Corneal Cyst
Written by Lee E. Moore, MD, Do Thuy Hang, MD, and Kenneth L. Cohen, MD. Photos by Dr. Cohen. Dr. Hang is at Vietnam National Institute of Ophthalmology, Hanoi, and Drs. Moore and Cohen are at the University of North Carolina, Chapel Hill.
An active, otherwise healthy 6-year-old girl presented with a “white spot” on her left eye that had been slowly growing over the past few years. She had not complained about her eye or shown signs of discomfort. Neither the girl nor her parents could remember any incidence of ocular trauma.
On examination, visual acuity (VA) was 20/25 and 20/200 in the right and left eyes, respectively. There was no afferent pupillary defect or strabismus. Slit-lamp biomicroscopy revealed conjunctival thickening inferonasally with vascularization encroaching upon the limbus in the left eye only. Adjacent to the limbus was an oval area of corneal thickening 6 mm wide by 5 mm high, extending from the limbus up into the visual axis (Fig. 1). The corneal stroma contained turbid fluid, with white material settling dependently (Figs. 1 and 2).
These findings suggested a corneal stromal cyst communicating from conjunctival epithelium as the result of a developmental or unrecognized traumatic etiology. The risk of amblyopia in a 6-year-old prompted surgical rather than conservative management.
We performed surgical incision and drainage through a partial-thickness clear corneal incision into the stromal cyst with a microkeratome blade. We applied 1.6% 5-fluorouracil for chemodestruction of the involved epithelial cells and then dissected conjunctiva away from the limbus to disrupt any potential communication with the corneal stroma. Cytological review of the cyst fluid revealed epithelial cells that were consistent with our clinical diagnosis. At her one-month postoperative visit, the patient’s VA had improved to 20/100 in the left eye; her cornea remained clear without recurrence (Fig. 3); and she was beginning treatment for amblyopia.
Read your colleagues’ discussion.
| BLINK SUBMISSIONS: Send us your ophthalmic image and its explanation in 150-250 words. E-mail to eyenet@aao.org, fax to 415-561-8575, or mail to EyeNet Magazine, 655 Beach Street, San Francisco, CA 94109. Please note that EyeNet reserves the right to edit Blink submissions. |