Download PDF
After 4 days of decreased vision in his right eye, Jimmy Greenhoff* presented to the emergency room. The 39-year-old denied any trauma or other inciting factors. He said that he had felt occasional right brow discomfort, but there had not been any eye pain, flashes, floaters, redness, discharge, or pain on eye movement. He also complained of occasional headache but denied fever, chills, joint pain, or rashes. He was concerned that his vision loss might be related to his 10-year history of neurocysticercosis. He stated that he had seen his neurologist 2 weeks earlier for a seizure, which was thought to be associated with new neurocysticercosis lesions seen on brain MRI.
Medical History
Mr. Greenhoff’s past medical history was significant for neurocysticercosis complicated by seizures, which had been diagnosed and treated in 2004 in Ecuador. He had been seizure free for 5 years until 2 weeks before our encounter.
His past ocular history included central serous chorioretinopathy in the left eye in 2010, which resolved spontaneously.
His active medications were albendazole, oxcarbazepine, and dexamethasone—all of which were prescribed for neurocysticercosis. He had no known drug allergies, and family history was noncontributory.
What We Saw
On examination, Mr. Greenhoff’s best-corrected visual acuity was 20/30 in his right eye and 20/60 in his left. His pupils were equally round and reactive without an afferent pupillary defect. Intraocular pressure was 11 mm Hg in both eyes; ocular motility was full.
Slit-lamp examination of the anterior segment of both eyes was unremarkable, with the exception of a 1-mm stromal scar nasal to the visual axis in the right eye. Dilated exam of both eyes revealed healthy-appearing optic nerves with a cup-to-disc ratio of 0.4. The macula appeared flat, and the vitreous was clear.
Examination of the peripheral retina in Mr. Greenhoff’s right eye revealed a white, round, flat subretinal lesion, approximately 1/3 disc diameter in size, just temporal to the arcades. There was no overlying vitritis or hemorrhage. Examination of the periphery of the left eye was unremarkable.
Clinical Course
We discussed our findings with a retina specialist and the patient’s neurologist, and no acute changes in clinical management were made.
Lab results. Laboratory analysis including complete blood count, metabolic panel, sedimentation rate, C-reactive protein, toxocariasis, and toxoplasmosis was performed; all results were within normal limits.
New findings at follow-up visit. At follow-up 2 days later, Mr. Greenhoff’s vision remained unchanged, as did his anterior segment examination. On repeat dilated fundus exam of the right eye, the once-flat subretinal lesion had become elevated and increased in size to approximately 2 disc diameters. Optical coherence tomography (OCT) of the lesion was performed. This showed an elevated cystic lesion that appeared to be migrating through the retina in the right eye. Fluorescein angiography revealed leakage from and around the lesion.
Our Diagnosis
It was apparent at this point that the most likely diagnosis of this large, white, cystic, migrating intraretinal lesion was an intraocular cysticercus cyst. We discussed treatment options with the patient and the need for surgical management in the near future; however, he wished to continue medical management and observation, despite the risks of vision loss, ocular inflammation, and worsening of his condition.
At follow-up 1 week later, Mr. Greenhoff had no change in vision or lesion size. Again, we discussed treatment approaches, as well as the option of laser demarcation of the lesion along with continued medical therapy, as the patient still resisted vitreoretinal surgery for lesion removal. With the understanding that the cysticercus would not be eliminated by laser demarcation and that his clinical condition could deteriorate by delaying vitreoretinal surgery, the patient underwent uneventful laser demarcation of the intraretinal lesion.
Despite multiple discussions with the patient regarding the necessity of surgery, he wished to continue medical therapy and observation, as his vision remained unchanged and he was not experiencing any eye pain or intraocular inflammation. Mr. Greenhoff remained stable for the following 3 weeks but, unfortunately, was lost to follow-up despite multiple phone calls and messages.
Discussion
Cysticercosis is caused by infection with the larval stage of the parasitic cestode Taenia solium.1 Humans are infected by eating food contaminated with feces. Once ingested, the oncospheres hatch in the intestine; invade the intestinal walls; and migrate to striated muscles, brain, liver, eye, and other tissues.1 Here, they develop into cysticerci.1,2
Geographic distribution. Although endemic to tropical areas (sub-Saharan Africa, India, East Asia, Latin America), U.S. incidence of cysticercosis is increasing as a result of immigration, increased travel to endemic areas, improved serologic testing, and availability of diagnostic imaging.3
Symptoms at presentation. The most common presentation of ocular cysticercosis is decreased vision, pain, and redness.2
Site of infection. In Western countries, the predominant site of involvement in ocular cysticercosis is subretinal.1 When the parasite is located in the subretinal space/vitreous, the proposed site of entry is choroidal vasculature, from which the cysticercus migrates into the subretinal space, bores a hole in the retina, and enters the vitreous cavity.2 Alternatively, the parasite may enter through the ciliary and retinal blood vessels.2
In some cases, the cyst develops in the anterior chamber, leading to iritis, secondary glaucoma, and anterior and posterior synechiae.2 Subconjunctival cysticercosis may induce a painful, yellowish nodule with surrounding congestion and possible spontaneous extrusion.2 Orbital cysticercosis may involve extraocular muscles, causing strabismus and ptosis.2 Lacrimal canalicular obstruction due to adnexal cysticercosis has also been reported.2
Workup. The workup for ocular cysticercosis includes enzyme-linked immunosorbent assay for anticysticercal antibody and complete blood count.2 Pars plana vitrectomy and/or retinotomy may be diagnostic and therapeutic but involves some risk.2 Imaging (brain and orbital CT/MRI) is important to identify any ocular lesions as well as to exclude lesions of neurocysticercosis.2,3 However, if neurocysticercosis is present, it is necessary to consult with neurology, infectious disease, and, occasionally, neurosurgery.3
Management approaches. The definitive management of intraocular cysticercosis is surgical. However, medical management and even laser have been used in certain circumstances.2 For extraocular muscle cysticercosis, antihelminthics (commonly praziquantel and albendazole) and oral corticosteroids have been found particularly effective.2
Medical management. Praziquantel induces destruction of approximately 75% of cysts with a single course.2 It has been found that, when combined with prednisone, praziquantel induces shrinkage and immobilizes intraocular cysticercus lesions within 3 days of therapy.4 However, this effect appears to be reversible—once therapy is discontinued, the parasite may regain motility and morphology.4
Albendazole is a broad-spectrum, cysticidal drug that destroys approximately 85% of cysts with a single course.2 Kim et al. described a case of subretinal cysticercosis treated with a tapering dose of albendazole and prednisone—they noted that in long-term follow-up (30 months after presentation), the subretinal lesion was less elevated, uveitis became quiescent, and vision improved.5
Corticosteroids (e.g., prednisone or dexamethasone) are typically used to help control inflammation resulting from the death of the intraocular organisms.2 However, it should be noted that use of medications in lieu of surgery is not without risk—patients may fail treatment or experience adverse effects.
Treatment in situ. Destruction of larvae in situ by photocoagulation, cryotherapy, and diathermy has been attempted with some success.2 Santos et al. state that small subretinal cysticerci (<8 mm, located away from macula) can be treated with xenon/ argon photocoagulation.6
Surgical removal. The most common approach to surgical removal is via pars plana vitrectomy, although transscleral removal of subretinal cysts located anterior to the equator may be performed.2 The cyst should be removed in toto and intact to reduce the potential for inflammation and to allow for best chance of good visual and functional recovery.2,6 Cysts located in the anterior chamber may be removed via paracentesis, extraction with forceps, cryotherapy, or viscoexpression through a small limbal incision.2
Follow-up. Patient education and follow-up are imperative to ensure resolution.3 The public must be taught about maintaining hand hygiene, washing raw produce before consumption, and avoiding raw or uncooked pork or other meat.3
Summary
The gold standard for treatment of intraocular cysticercosis is surgical removal, with careful avoidance of inducing intense intraocular inflammation, which can lead to blindness, phthisis, and loss of the eye. However, our experience with Mr. Greenhoff, who declined surgical intervention, suggests that there may be utility in medical management and laser demarcation to halt, or slow, lesion migration through the retina. Perhaps this example may be useful in other cases where patients may not be good candidates for vitreoretinal surgery or do not have access to proper surgical care.
___________________________
*Patient name is fictitious.
___________________________
1 Li JJ et al. Korean J Parasitol. 2013;51(2): 223-229.
2 Menon-Mehta S. Ocular cysticercosis. http://emedicine.medscape.com/article/1204683-overview. Accessed July 6, 2015.
3 Centers for Disease Control and Prevention. Cysticercosis. www.cdc.gov/parasites/cysticercosis/. Updated April 2014. Accessed July 6, 2015.
4 Kestelyn P, Taelman H. Br J Ophthalmol. 1985;69(10):788-790.
5 Kim W, Chee S. Retina. 2004;24(3):469-471.
6 Santos R et al. Ophthalmology. 1979;86(8):1501-1504
___________________________
Dr. Nattis is a chief resident in ophthalmology, Dr. Mahdavi is a second-year ophthalmology resident, and Dr. Josephberg is an associate professor of ophthalmology and chief of the retina service; all 3 are at New York Medical College in Valhalla. Relevant financial disclosures: None.
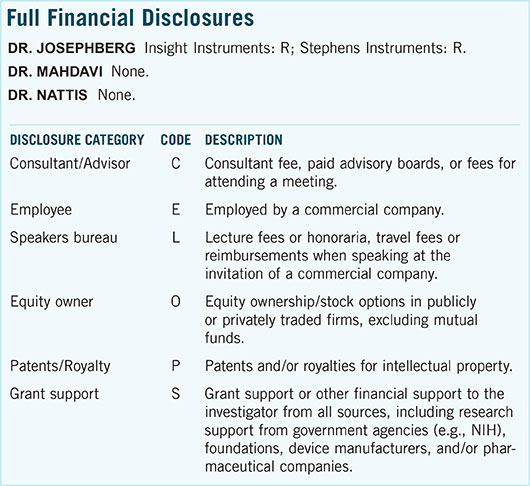
For full disclosures and the disclosure key, see below.