This article is from March 2006 and may contain outdated material.
Eyes that are dry, burning, itchy and have excessive tearing and sensitivity to light—these are all patient complaints that are heard in ophthalmology practices daily. While most commonly associated with older age and lower tear production, dry eye syndrome can also be associated with rheumatoid arthritis, lupus and similar diseases. It can also result from thermal or chemical burns. It often occurs in people who are otherwise healthy.
Coding for the treatment of this irritation varies by payer. A common documentation requirement is the chief complaint, which is similar to those provided in the opening sentence. You also should document gland deficiency, as shown, for example, on a Schirmer test. Also include a statement that traditional methods, such as artificial tears and/or ointment, have not been successful.
Punctal Occlusion
Two CPT codes focus on the closure of the puncta. One is code 68760 Closure of the lacrimal punctum; by thermocauterization, ligation or laser surgery. This has a 10-day global period. Typical Medicare allowable is $194 when performed in the office and $125 in a facility.
A more common procedure is code 68761 Closure of the lacrimal punctum by plug, each. This carries a 10-day global period. Typical Medicare allowable when performed in the office is $133 and in a facility $93. The same CPT code is used when coding temporary (collagen) and permanent (silicone) plugs. You don’t have to distinguish the difference to the payer.
In 2002, Medicare bundled the supply of the plug with the insertion. You should not bill the supply of the plug to Medicare or the Medicare beneficiary.
When there is a separately identifiable service the same day as the insertion of the plug(s), modifier –25 significant, separate service same day as minor procedure should be appended to the appropriate level of E&M or Eye Code.
When occluding the two lower puncta, use CPT code 68761–E2 and code 68761–E4 for Medicare patients.
Covered diagnosis codes include:
- 370.20 Superficial keratitis, unspecified
- 370.21 Punctate keratitis, Thygeson’s superficial punctate keratitis
- 370.33 Keratoconjunctivitis sicca, not specified as Sjögren’s
- 370.34 Exposure keratoconjunctivitis
- 372.53 Conjunctival xerosis
- 375.15 Tear film insufficiency, unspecified dry eye syndrome
- 375.52 Stenosis of lacrimal punctum
- 375.56 Stenosis of nasolacrimal duct, acquired
- 710.2 Sicca syndrome (keratoconjunctivitis sicca, Sjögren’s disease)
The Correct Coding Initiative (CCI) bundles the following CPT procedures with punctal occlusion: 36000, 36410, 37302, 62318, 62319, 64402, 64416, 64417, 64450, 64470, 64475, 67500, 68440, 68705, 68770, 68801, 69990, 90760, 90765, 90772, 90774, 90775, 90780, C8950, C8952 and J2001.
 |
|
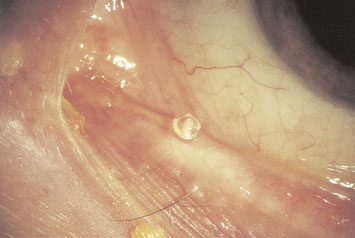
The punctal plug provides relief for dry eye patients—but how do you ensure that you get reimbursed appropriately?
|
What about non-Medicare payers? Most non-Medicare payers will not pay for an exam the same day as punctal occlusion even with modifier –25. They bundle the exam with the procedure.
Most non-Medicare payers do not recognize the –E modifiers. They do recognize modifiers –50 and–51.
Most non-Medicare payers will pay for the supply of the punctal plugs: Use HCPCS codes A4262 for collagen plugs and A4263 for silicone plugs. If the payer doesn’t recognize HCPCS codes, use the supply code 99070. List punctal plugs as the supply in the free-form text area of the HCFA 1500 claim form. You may have to attach an invoice showing your cost for the supply of the plugs.