By Trisha Sharma, MBBS, and M. Manjunath Kamath, MBBS, DOMS, MS
Edited by Sharon Fekrat, MD, and Ingrid U. Scott, MD, MPH
Download PDF
Orbital lymphoma is a type of non-Hodgkin lymphoma (NHL) that originates in the conjunctiva, lacrimal gland, soft tissues of the eyelid, or extraocular muscles; it is most commonly extraconal in location. Orbital lymphoma is said to be primary when it arises spontaneously from one of these locations, and secondary when it is associated with metastatic spread from an extraorbital site.
Epidemiology
While lymphoma constitutes more than half of all orbital malignancies (55 percent),1 the incidence of orbital lymphoma has been reported to account for between 1 and 10 percent of NHL cases.2
Orbital lymphoma may be unilateral or bilateral. Although it has been known to present in patients between 15 and 70 years of age, most cases cluster around the seventh decade. Historically, a female preponderance has been noted,3 but there have been several conflicting reports regarding gender predominance. Geographically, the disease is most common in Asia and Europe.
Pathophysiology
Immunosuppression due to any cause—including AIDS, immunosuppressive drugs, or increasing age—has long been established as the main factor contributing to the pathophysiology of orbital lymphoma.
More recently, however, the role of various pathogens has entered into the debate. These include associations with Chlamydia psittaci and Helicobacter pylori, as well as some viruses.
Histology
Almost 80 percent of orbital and adnexal lymphomas are of low-grade variety, with B-cell lymphomas and extranodal marginal zone lymphoma of the mucosa-associated lymphoid tissue type (MALT lymphoma) being the most common histological diagnoses.4 MALT lymphomas comprise a distinct set of tumors that exhibit the unique property of “homing,” which permits lymphoma cells to adhere to other epithelial and mucosal sites, thus enabling bilateral involvement.
Other subtypes have also been reported, including follicular lymphomas, diffuse large B-cell lymphomas, and mantle cell lymphomas.
Clinical Presentation
The clinical presentation is generally nonspecific and depends on the location of the lymphoma. Vision is usually preserved, as infiltration of the globe or optic nerve is rare.
Conjunctiva. Patients typically demonstrate a pink or red “salmon patch” of swollen conjunctiva or conjunctival hyperemia.
Orbit. Orbital presentation is most commonly observed as a painless palpable mass in the superolateral quadrant. It may lead to proptosis, ptosis, diplopia, or abnormal ocular movement.
Lacrimal gland. The enlarged gland displaces the eyeball inferomedially.
Eyelids. Swelling and prolapse may occur in the eyelid.
Diagnosis
The differential diagnosis of orbital lymphoma includes the following:
- Pseudotumor
- Orbital metastases
- Diffuse lymphangioma
- Lacrimal adenoma
- Cavernous hemangioma
- Lymphoid lesions of the orbit (benign reactive lymphoid hyperplasia, atypical lymphoid hyperplasia)
Diagnostic workup. The following evaluations form the basis of a good diagnostic workup, undertaken in conjunction with the patient’s internist:
- History and physical examination
- Dilated fundus examination
- Thorough examination of opposite orbit as well as the oral cavity and oropharynx
- Complete blood count, biochemistry profile
- Fine-needle aspiration and biopsy
- Liver function tests, renal function tests
- Chest x-ray
- Computed tomography (CT) and magnetic resonance imaging (MRI) of orbit, abdomen, thorax, and pelvis
- Bone marrow aspiration
Imaging
Computed tomography. The typical finding on CT scanning is a moderately well-defined orbital mass, which molds to the adjacent ocular structures without bony destruction. It is usually homogeneous in density, either isodense or slightly hyperdense when compared with the density of the extraocular muscles. It may exhibit any of the following four patterns: retroocular, anterior preseptal, lacrimal gland involvement, or extension of an adnexal lesion.
Lesions that are heterogeneous, with bony destruction, are indicative of high-grade lymphomas, which are usually accompanied by pain.
Magnetic resonance imaging. Compared with the extraocular muscles, the orbital mass appears isointense or hypointense on a T1-weighted MRI scan, but it appears isointense to hyperintense on a T2-weighted scan. Hypointense T2-weighted images are suggestive of high-grade lymphomas.
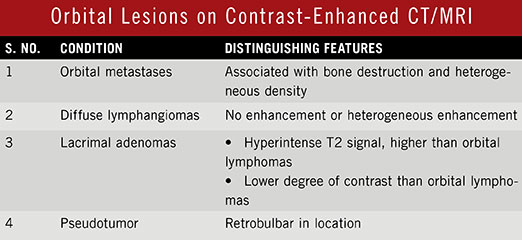
Contrast-enhanced imaging techniques. Contrast-enhanced CT/MRI scans reveal mild to moderate enhancement of the lesion, and when this is seen in T1-weighted images, high cellularity of the lymphoma can be expected. High cellularity in lymphoma produces a lower apparent diffusion coefficient (ADC) of <0.1 × 10-3. This differentiates it from other types of expansive orbital lesions.
Spiral CT. Another radiological investigation that may be helpful is spiral CT using dual-phase contrast enhancement. Lymphoma may display decreased density on delayed images, thus differentiating it from orbital pseudotumor, which shows increasing density on delayed images. (See Web Extra, “Orbital Lesions on Contrast-Enhanced CT/MRI.”)
Dynamic contrast-enhanced MRI. Dynamic contrast-enhanced MRI scans may be performed to distinguish lymphomas from other conditions. Studies of contrast index curves of orbital lymphomas exhibit a characteristic steep rise followed by a rapid decline.
|
Web Extra: Pearls
|
 |
Treatment and Prognosis
There are four main treatment options for orbital lymphoma: surgery, radiotherapy, chemotherapy, and immunotherapy. Prognosis depends upon the histology, grade and stage (see “Grading and Staging”), and treatment modality employed, but the overall five-year survival rate is approximately 60 percent.
Grading and Staging
Grading
Grade describes the aggressiveness of the disease.
- Low grade. Indolent or slow growth rate
- Intermediate grade. Moderate growth rate
- High grade. Aggressive or rapid growth rate
Staging
Orbital lymphomas are staged according to the Ann Arbor system.
- Stage I. Confined to the orbit
- Stage II. Involvement of adjacent structures such as the sinuses, tonsil, and/or nose
- Stage III. Abdominal nodal disease below the diaphragm
- Stage IV. Disseminated involvement of one or more extranodal sites, such as liver or bone
Suffixes
The following letters are added to provide more specific information.
- E. Used when there is local extranodal extension (e.g., IE, IIE, IIIE, IVE).
- A. No symptoms
- B. Fever (temperature higher than 38°C), drenching night sweats, and unexplained loss of more than 10 percent of body weight within the preceding six months.
|
Surgery
Surgery plays a dual role in the management of orbital lymphomas, being both diagnostic and therapeutic. However, although biopsy is important for accurate diagnosis, surgery as the sole treatment modality often ends with a much-dreaded relapse of disease. This is probably because the location of the tumor makes it difficult for the surgeon to achieve both complete excision and preservation of ocular function and aesthetics.
Radiotherapy
Because most orbital lymphomas are localized, radiotherapy is the most common and preferred treatment modality. The entire orbit must be encompassed in the radiation field, irrespective of how much of the orbit is involved. This reduces the chance of recurrence in previously uninvolved areas.
Doses of 25 to 35 Gy are considered to be curative for low-grade tumors, and 30 to 40 Gy for the high-grade varieties. However, the higher doses, especially greater than 35 Gy, are associated with significant complications. These include
- Conjunctivitis and dry eye, which are the most common acute side effects.
- Keratitis and corneal ulceration.
- Cataract, which is the most frequent delayed consequence of radiation to the orbit. Lens shielding can substantially reduce the incidence of radiation-induced cataract and should be used in cases where it does not compromise complete coverage of tumor.
- Radiation retinopathy.
Recurrences can be treated by either surgery or repeat radiation.
Chemotherapy
Chemotherapy has a limited role in the definitive treatment of orbital lymphomas. Currently, there is no indication for use of chemotherapy in solitary orbital lymphomas, except in diffuse large B-cell lymphoma. It is usually reserved for tumors categorized as stage II or higher, especially advanced stages like III and IV. It may be administered either after surgery or in combination with radiation. Chemotherapy may be given as a single agent or as combination therapy. Consultation with an oncologist is necessary.
Monotherapy. Alkylating agents such as cyclophosphamide are typically used.
Oral chlorambucil has been used as a monotherapy for MALT lymphoma, at a mean total dose of 600 mg. A complete response of almost 80 percent has been reported. It has minimal side effects and is well tolerated, even by elderly patients.5 However, recurrence rates are high.
Combination therapy. Regimens containing doxorubicin are preferred, such as CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone or prednisolone) and CVAD (cyclophosphamide, vincristine, doxorubicin, and dexamethasone). Significant side effects include myelosuppression and congestive heart failure.
Immunotherapy
Neoplastic cells of MALT lymphomas have been shown to express the antigen CD20 on their surfaces. Rituximab is a chimeric monoclonal antibody that is directed against CD20, ultimately leading to cell destruction by various mechanisms including apoptosis, complement-mediated cytolysis, and antibody-dependent cytotoxicity.
The major drawback of monotherapy with rituximab is a high rate of relapse.6 Initially, the standard induction therapy was four weekly cycles of rituximab at doses of 375 mg/m2 administered as intravenous infusion.7 However, to overcome the problem of recurrence, an additional maintenance regimen of treatment every two months for two years has been proposed.8
Reported side effects include nausea, fever, and pruritus; rarely, bronchospasm, anaphylaxis, and hypotension may occur.
Recently, combination therapy consisting of rituximab and chlorambucil has shown promising results in newly diagnosed cases of orbital lymphoma.
Other Therapeutic Options Antibiotics. Oral doxycycline has been used for treatment in cases of orbital lymphoma that were positive for C. psittaci DNA. It shows a response rate of about 48 percent.7
Radioimmunotherapy. In this modality, a monoclonal antibody is administered with a radioactive ligand. Although some antigen-negative tumor cells may be missed by immunotherapy, they are destroyed by the beta particles emitted during radiation, allowing lysis of such cells by radioactive cross-fire from neighboring antigen-positive antibody–coated cells.
Follow-up Treated patients require lifelong follow-up to monitor for complications and to detect recurrence and secondary tumor formation. Visits may be scheduled once every three months for two years, then every six months for the subsequent three years, and then every year. Each visit should include a complete history, physical examination, and radiological investigations, if indicated.
___________________________
1 Margo CE, Mulla ZD. Ophthalmology. 1998;105(1):185-190.
2 Eckardt AM et al. World J Surg Oncol. 2013;11:73.
3 Ahmed S et al. Am J Med Sci. 2006;331(2):79-83.
4 Fung CY et al. Int J Rad Oncol Biol Phys. 2003;57(5):1382-1391.
5 Ben Simon GJ et al. Ophthalmology. 2006;113(7):1209-1213.
6 Ferreri AJ et al. Haematologica. 2005;90(11):1578-1579.
7 Stefanovic A, Lossos IS. Blood. 2009;114(3):501-510.
8 Ardeshna KM et al. Lancet Oncol. 2014;15(4):424-435.
___________________________
Dr. Sharma is a resident in ophthalmology, and Dr. Kamath is professor of ophthalmology at Kasturba Medical College, Mangalore, Karnataka, India. The authors report no financial interests.