By Maya S. Ling, MD, and Rona Z. Silkiss, MD, FACS
Edited by Sharon Fekrat, MD, and Ingrid U. Scott, MD, MPH
Download PDF
Sebaceous carcinoma of the eyelid is a rare but potentially fatal neoplasm that represents approximately 5 percent of malignant eyelid tumors. Its incidence varies depending on demographics, ranging from 0.5 per million in Caucasians age 20 and older1 to higher rates in Asian populations, with one review from India reporting that 28 percent of 85 malignant eyelid tumors were sebaceous cell carcinoma.2
The condition is known as the “great masquerader,” as it is often mistaken for a benign or a different malignant lesion. This leads to a delay in diagnosis and contributes to an increase in associated morbidity and mortality.
Although earlier series described mortality rates of 18 to 30 percent, more recent reports suggest improved survival rates, perhaps as a result of increased awareness and earlier detection of the disease.3
Pathogenesis
Sebaceous carcinoma of the eyelid appears to develop de novo and not from a sebaceous adenoma, sebaceous hyperplasia, or sebaceous nevus. The disease arises from the sebaceous glands of the periocular region, which include the meibomian glands, Zeis glands, and glands present in the caruncle and conjunctiva.
Several studies have suggested that mutations in the gene for the tumor suppressor protein p53 may be involved in the underlying pathogenesis of the disease.
Presentation and Risk Factors
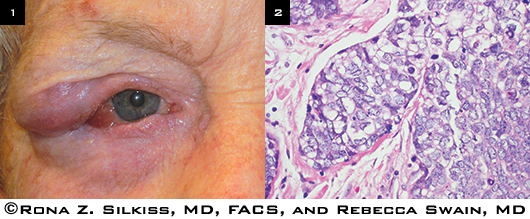
Sebaceous carcinoma of the eyelid can present in a variety of ways, but the most common variants are either a solitary eyelid nodule (Fig. 1) or diffuse eyelid thickening, sometimes with loss of cilia.
Risk of misdiagnosis. The condition is notorious for being misdiagnosed as a persistent or recurring chalazion or blepharitis, leading to an average delay of one to three years before the correct diagnosis is established. It is important for clinicians to consider sebaceous carcinoma in middle-aged or older patients who present with unilateral blepharitis. Less commonly, sebaceous carcinoma can grow outward, becoming a pedunculated lesion; occasionally, it can ulcerate and resemble basal cell carcinoma.
Occasionally, primary sebaceous carcinoma develops in the lacrimal gland. No matter the site of origin, sebaceous carcinoma can spread through the entire eyelid and invade the orbit.
Contributing risk factors. The condition is generally seen in older individuals, and the mean age at diagnosis ranges from the late 50s to the early 70s. However, sebaceous carcinoma may present in younger patients, especially if they have a history of facial or ocular irradiation or immunosuppression. Most studies have found a female predominance, and there is a well-known higher incidence among Asians. Sebaceous carcinoma may be associated with Muir-Torre syndrome.4
 |
|
PRESENTATION AND HISTOPATHOLOGY. (1) Patient with recurrent, advanced sebaceous carcinoma in the upper right eyelid that has infiltrated the lower lid. (2) The tumor specimen of this patient shows finely vacuolated cytoplasm.
|
Diagnosis and Management
The initial goals of management are to diagnose the disease and determine the extent of its spread.
Differential diagnosis. In addition to blepharitis and chalazion, the differential diagnosis for sebaceous carcinoma of the eyelid includes basal cell carcinoma, lymphoma, melanoma, Merkel cell carcinoma, and squamous cell carcinoma. Chalazion generally occurs in younger patients and is often tender and circumscribed; blepharitis is usually bilateral. In most cases, neither is associated with loss of cilia. Basal cell carcinoma is usually found in the lower eyelid and is often a white or translucent lesion with vascular edges and ulceration. (Ulceration is rare in sebaceous carcinoma, which is more commonly found in the upper eyelid.) Squamous cell carcinoma is more common in the upper eyelid but is generally associated with actinic keratosis of the facial skin.
Biopsy. Full-thickness incisional or excisional biopsy of the eyelid lesion should be performed, followed by histopathologic analysis. Lesions have distinctive cytologic features, characterized by finely vacuolated cytoplasm and high mitotic activity (Fig. 2). Lipid within the tumors may cause a giant cell reaction that can be mistaken for a chalazion. A common characteristic of sebaceous carcinoma is pagetoid spread, involving intraepithelial extension into the eyelid epidermis and conjunctival epithelium. A number of immunohistochemical stains have been reported to aid in differentiating sebaceous carcinoma from more common neoplasms.
As sebaceous carcinoma is a rare disease, an incorrect initial pathologic diagnosis—most commonly squamous cell or basal cell carcinoma—has been reported in 40 to 75 percent of cases, often when specimens have been analyzed by an inexperienced pathologist.3 Thus, it may be prudent to have an ocular pathologist review biopsy sections if the initial pathologic diagnosis is negative for sebaceous carcinoma but clinical suspicion remains high.
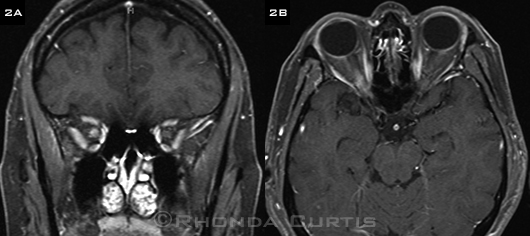
Examination. A comprehensive physical exam to assess the globe and the periocular region for disease as well as palpation of the preauricular and cervical areas for enlarged lymph nodes should be performed. If the eyelid lesion appears to be diffuse or if there is any evidence of lymphadenopathy, then orbital or systemic imaging is warranted to evaluate the degree of disease spread (Figs. 3 and 4). Fine-needle aspiration biopsy of suspicious lymph nodes has been used to diagnose sebaceous carcinoma.
Surgical excision. Eyelid tumors should be treated initially with primary surgical excision. Frozen sections or Mohs surgery is often used intraoperatively to assess the margins of the lesion for residual tumor, with additional resection continuing until there is histopathologic confirmation of clear margins. Although prompt intraoperative evaluation for residual tumor is convenient, these methods may not be completely reliable because sebaceous carcinoma can have patchy epithelial involvement with skip areas. Several cases have been reported in which surgical margins were deemed free of disease, but residual carcinoma was still detected in the paraffin-embedded permanent sections. As a result, some authors support a greater reliance on permanent sections for diagnosis.5 In addition, conjunctival map biopsies are often advocated in order to help determine the extent of disease and plan for definitive treatment.
Exenteration. In the past, conjunctival involvement or spread of sebaceous carcinoma was considered an indication for exenteration. With improvements in eyelid and conjunctival reconstruction using rotational skin flaps and grafting, exenteration is generally reserved for cases of unresectable orbital disease in the absence of distant metastasis.
Adjunctive therapy. Cryotherapy may be used for both eyelid and conjunctival sebaceous carcinoma. More recently, topical chemotherapy in the form of mitomycin C has been advocated in cases of pagetoid invasion of the conjunctiva. Most authors do not believe that radiation should be used for primary treatment, but it may have a role in patients who decline surgical excision or exenteration.
 |
|
EVALUATING DISEASE SPREAD. Magnetic resonance imaging shows a 2.5 x 1.6 x 2.1 cm mass lateral to the right orbit that enhances postgadolinium.
|
Prognosis
Factors that have been associated with a worse prognosis include localized or distant metastasis, orbital invasion, involvement of upper and lower eyelids or multicentric origin, poor differentiation, tumor diameter exceeding 10 mm, and pagetoid invasion.6
Metastasis. The most frequent sites of local metastasis are the preauricular, parotid, and cervical lymph nodes. If there is evidence of regional metastasis on imaging or physical exam, lymph node dissection should be considered. As surgeons have gained more experience with sentinel lymph node biopsies, the rates of false-negative results have begun to decrease. However, because sebaceous cell carcinoma is relatively rare, most of the data related to lymph node biopsies come from small cohorts. Therefore, sentinel lymph node biopsies have not yet been established as a routine method of evaluation in patients with sebaceous carcinoma.7 The most common sites of distant metastases are the liver and lung. Systemic chemotherapy, guided by an oncologist, may be warranted in cases of metastatic disease.
Staging. In one study, researchers showed that tumor size, the main determinant of the “T” category of the American Joint Committee on Cancer TNM staging system for eyelid carcinoma, correlated with lymph node metastasis and disease-specific survival in a group of 50 patients with sebaceous carcinoma of the eyelid. Category T2b (tumor size of 10 to 20 mm or involvement of full-thickness eyelid) or worse correlated with regional lymph node metastasis. Category T3a (tumor size greater than 20 mm or invasion of local ocular or orbital structures, or perineural invasion) or worse correlated with distant metastasis and death. Overall rates of nodal metastasis vary but may be present in up to 18 percent of cases. Five-year disease-specific survival rates also vary, ranging from 79 to 97 percent.8
Conclusion
It is important for clinicians to be familiar with the varied presentations of sebaceous carcinoma of the eyelid so that patients receive prompt diagnosis and treatment of a potentially fatal disease.
___________________________
1 Margo CE, Mulla ZD. Arch Ophthalmol. 1998;116(2):195-198.
2 Abdi U et al. J Indian Med Assoc. 1996;94(11):405-409, 416, 418.
3 Shields JA et al. Surv Ophthalmol. 2005;50(2):103-122.
4 Gaskin BJ et al. Br J Ophthalmol. 2011;95(12):1686-1690.
5 Song A et al. Ophthal Plast Reconstr Surg. 2008;24(3):194-200.
6 Rao NA et al. Hum Pathol. 1982;13(2):113-122.
7 Pfeiffer ML et al. Ophthal Plast Reconstr Surg. 2013;29(1):57-62.
8 Esmaeli B et al. Ophthalmology. 2012;119(5):1078-1082.
___________________________
Dr. Ling is a third-year ophthalmology resident, and Dr. Silkiss is chief of ophthalmic plastic, reconstructive, and orbital surgery; both are at the California Pacific Medical Center in San Francisco. The authors report no related financial interests.