DMEK Versus Ultrathin DSAEK for Corneal Endothelial Dysfunction
By Lynda Seminara
Selected By: Stephen D. McLeod, MD
Journal Highlights
Ophthalmology, January 2019
Download PDF
Results of nonrandomized and observational studies have suggested that visual outcomes are similar for Descemet membrane endothelial keratoplasty (DMEK) and ultrathin Descemet stripping automated endothelial keratoplasty (UT-DSAEK). However, the study designs have hindered direct comparisons. To permit a more meaningful comparison of these procedures, Chamberlain et al. conducted a randomized controlled trial to evaluate visual outcomes and complication rates. They found that DMEK yielded superior visual acuity during the year following surgery, although complication rates were similar for the two procedures.
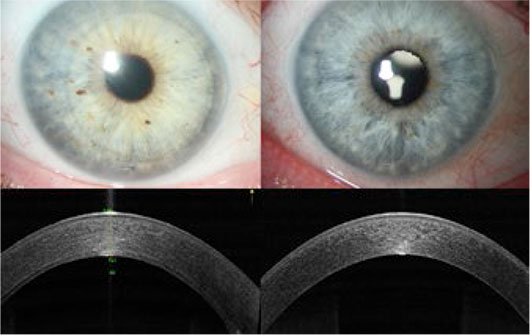 |
COMPARISON. Clinical photographs and OCT images from patients who underwent UT-DSAEK (left) and DMEK (right).
|
Eligible participants had damaged or diseased endothelium (from Fuchs endothelial dystrophy or pseudophakic bullous keratopathy). Within two days prior to surgery, eyes were assigned randomly to receive DMEK or UT-DSAEK. Standardized surgical techniques were used. Patients were masked as to their intervention and received the same postoperative instructions. Moreover, the refractionist who assessed visual outcomes was unaware of each patient’s procedure. The primary out-come was best spectacle-corrected visual acuity (BSCVA) at six months. Secondary outcomes were BSCVA at the three- and 12-month marks, intra- and postoperative complications, endothelial cell counts, and change in pachymetry.
Of the 216 patients with endothelial dysfunction who were screened, 38 (50 eyes) were enrolled. After the researchers corrected for baseline VA, DMEK was found to result in better visual outcomes. BSCVA was 1.5 lines better for the DMEK group at three months, 1.8 lines better at six months, and 1.4 lines better at 12 months. At six months, the average endothelial cell count was 1,963/mm2 in the DMEK group and 2,113/mm2 in the UT-DSAEK group. At 12 months, the average cell counts were 1,855/mm2 and 2,070/mm2, respectively.
Rates of intra- and postoperative complications were comparable for the study groups.
The authors noted that DMEK—when performed by experienced surgeons—appears to elicit better visual outcomes and faster recovery than UT-DSAEK. They emphasized that larger multicenter trials may help to clarify the dissimilar outcomes. (Also see related commentary by Marianne Price, PhD, in the same issue.)
The original article can be found here.