News in Review
First U.S. Guidelines for Retinoblastoma Screening
Download PDF
A panel of ophthalmic oncologists, pathologists, and geneticists has published the first set of U.S. screening guidelines for children at risk for retinoblastoma—the most common eye tumor affecting children.1
The goal. The team from the American Association of Ophthalmic Oncologists and Pathologists met over the course of 2 years to identify the key problems and clinical discrepancies in approaching “at-risk” patients—that is, children with a family history of retinoblastoma in a parent, sibling, or first- or second-degree relative. The published consensus report is a consolidation of how to proceed in different scenarios to initially identify and stratify disease risk and then follow up with these patients.
“The ultimate goal is that all children at risk for retinoblastoma are diagnosed as early as possible and followed up appropriately to treat tumors when they are very small and manageable with local therapies,” said coauthor Patricia Chévez-Barrios, MD, at Houston Methodist. “The treatment itself will vary depending on tumor size and location and other features in the eye, and it’s at the discretion of the treating team to decide which approach is indicated once the diagnosis is made.”
The recommendations. Highlights of the report include the following:
- All children with a family history of retinoblastoma should receive counseling and testing to clarify disease risk.
- The frequency of dilated fundus examination should be stratified on the basis of age and risk. Newborns at high risk, for example, require more frequent examination, every 2 to 4 weeks during their first 2 months of life. Newborns at intermediate or low risk should undergo monthly examination.
- Exam frequency declines as the child grows older, but screening for all at-risk patients should occur up to age 7. For asymptomatic children, no further screening is recommended after this time unless they are known to carry an RB1 These individuals should be followed indefinitely, every 1 to 2 years.
- All decisions regarding examination method should be discussed with the child’s family. Anesthesia is strongly recommended for any child unable to participate in a thorough in-office exam.
- Examiners should also be aware that tumor location can be age-specific. Newborns may present with tumors in the posterior pole; however, in children who are older at the time of disease development, the tumor may present peripherally.
Multispecialty support. The report has been endorsed by the Academy’s Quality of Care Secretariat as well as several medical organizations.
—Mike Mott
___________________________
1 Skalet AH et al. Ophthalmology. Published online Oct. 18, 2017.
___________________________
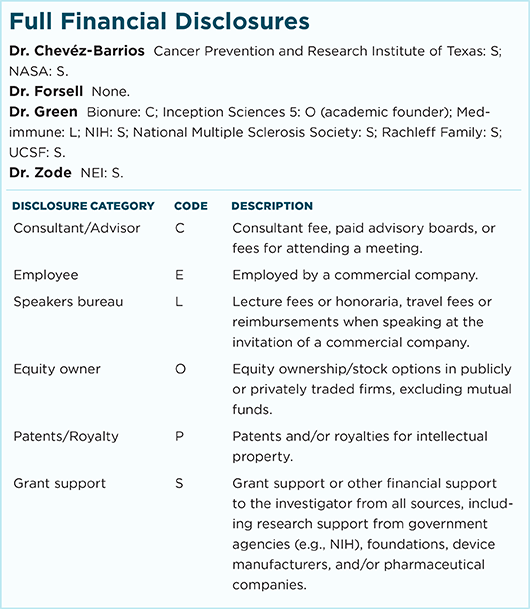
Relevant financial disclosures—Dr. Chévez-Barrios: None.
For full disclosures and disclosure key, see below.
More from this month’s News in Review