By Leslie Burling-Phillips, Contributing Writer, interviewing Denise C. Fridl, COT, COE, CPPM, OCS, Dennis P. Han, MD, Aneesh Suneja, MBA, and Joy Woodke, COE, OCS
Download PDF
The ability to reduce wait times without rushing the physician from patient to patient is the holy grail of patient satisfaction. This can be achieved by applying lean principles of practice management and removing the many and varied sources of waste from the health care delivery process,” said Aneesh Suneja, MBA, who is coauthor of Lean Doctors and founder of FlowOne Lean Consulting.
Why you should focus on wait times. “Wait times are a highly visible indicator of our performance. No other metric tells us the state of our process so clearly,” said Mr. Suneja. Furthermore, long wait times are a primary driver of patient dissatisfaction. (While Part 3 of this EyeNet series focuses on wait times, Part 1 introduced some key lean principles, such as the value stream, and Part 2 focused on the waste walk and the 5S method for evaluating and improving processes.)
Identify the Problems
“We used value stream mapping to determine what changes should be made,” said Dennis P. Han, MD, director of the vitreoretinal service at the Medical College of Wisconsin. As part of value stream mapping, you identify what is of value to a patient. Activities that directly contribute to that value are considered “value-added activities”; those that don’t are considered waste, and you should strive to eliminate them. Dr. Han and his staff went lean about 5 years ago under Mr. Suneja’s guidance—and experienced an 85% decrease in patient wait times.
Perform a “waste walk.” “Our entire staff followed a mock patient throughout a clinical encounter and measured wait times between value-added activities,” said Dr. Han. This procedure, known as a waste walk, enabled his staff to identify many underlying causes for delays and helped everyone to understand the entire process. “When everyone has a common understanding of the process, it becomes a team effort. Everybody can see how they are interlinked to produce better patient care and satisfaction. As a result, there is no longer finger- pointing,” said Dr. Han.
The goal is to improve patient flow. Ideally, patients would move from one step of their visit to the next without any delays. But there are many factors that can interrupt patient flow, including scheduling problems (e.g., patients arriving late and patient emergencies), bottlenecks (e.g., waiting for equipment to become available), and other inefficiencies (e.g., supplies or equipment are stored far from point of use).
Perceptions Matter
Believe it or not, your waiting room’s appearance can affect patients’ perception of wait time. Ms. Woodke’s practice, for example, has 2 locations, and patients typically have the exact same wait time in both clinics. However, she said, “our new office is much larger, and our patients at that clinic have reported that they thought they did not wait as long, presumably because it did not feel so crowded, loud, and chaotic. When a patient walks into a full waiting room, they already think that you are behind, whether you are or not.”
How to change perceptions. Removing clutter can make your waiting room seem less cramped. You also can move some patients to a sub-waiting room. And Ms. Woodke recommends keeping patients occupied. “In my experience, patient satisfaction increases the more that you distract them from the waiting process. We have TVs in all our rooms, with the same program playing, so as they transition through the flow, they are able to continue the story during the next step.”
|
Look for Solutions
Once you and your staff start recognizing the impediments to smooth patient flow, you’ll start looking for solutions. Here are some of the changes that proved successful for 3 practices.
Reallocate tasks. When Asheville Eye Associates in North Carolina conducted their value stream analysis, they noted that patients were waiting in line at the end of their exam to make payments and appointments. “To solve this problem, we moved collections to a pre-exam activity and moved the posting of charges and appointment follow-up scheduling to the end of an exam. These tasks are now completed by our technicians,” said practice administrator Denise Fridl, COT, COE, CPPM, OCS. By making minor changes in its processes, the practice eliminated several positions and increased its patients’ satisfaction.
Address bottlenecks. In a retina practice, patient flow slows in the photography and image acquisition areas, said Dr. Han. “To solve this problem, we moved our OCT imaging devices into the examination area.” (They had been located in a distant part of the clinic.) “This reduced the steps that had to be made by both my staff and my patients and improved our patient flow.”
Take advantage of technology. “Scanning insurance cards versus copying them, although a small modification, can make a big difference in practice flow,” said Joy Woodke, COE, OCS, practice administrator at Oregon Eye Consultants in Eugene. “We have also embraced using our patient portal. Patients are able to register online, receive confirmations, and cancel appointments, for example, which has streamlined multiple processes and measurably improved our flow.”
Focus on changeover processes. The lean approach distinguishes between “value-added processes” and “changeover processes.” Physician-patient interaction provides value to a patient and, thus, is considered a value-added process. In contrast, changeover processes include tasks that need to be done as the physician moves from one patient to the next, such as getting the chart ready for the next patient, dilating eyes, and moving patients in and out of the exam room.
When the changeover processes are performed by the physician, it extends the time between value-added processes. Instead, whenever possible, these changeover processes should be handled by staff in parallel to a physician’s processes so that the physician is able to efficiently move from one patient to the next and devote every minute to hands-on health care, said Dr. Han. For example, Dr. Han’s practice stopped moving patients in and out of the exam room. “This reduced the amount of time that people were going to the waiting room and back in to the exam area. Our patients are screened by a technician, their pupils are dilated, and they are seen by a physician—all in one exam room. And while one patient’s eyes are being dilated, the team moves to the next exam room and repeats the process, so there is always a patient ready to see a physician. This considerably reduced the amount of time spent walking around needlessly for everyone,” he said.
Similarly, at Asheville Eye Associates, they “strive to have 2 workup rooms and 2 physician rooms per clinic. This allows for the system to move patients efficiently,” said Ms. Fridl. “This was also the smallest change we made that resulted in the greatest impact on wait times. Our patients do not feel they are waiting excessively because something is always being done.”
Deputize staff to troubleshoot problems with patient flow. “In each of our clinics, we assign ‘facilitators’ (usually a scribe) to work with a particular physician on certain days,” said Ms. Woodke. “These are our ‘traffic directors,’ and they ensure that our clinical traffic is moving fluidly. If one of our technicians gets behind and is not loading the rooms or working up a patient quickly enough, the facilitator assists with getting them back on schedule.”
Improve Scheduling
If too many patients are scheduled in the morning or immediately after lunch, delays can occur, which can cause a domino effect of dissatisfaction throughout the clinic.
Allow flexibility. Paying close attention to the type of patient visit and allowing time for the unexpected are critical to keep the flow moving. “Within our retina practice, 1-month follow-up appointments tended to take up every single slot in our schedule,” said Ms. Woodke. “Now, we always leave room for consultations and emergencies. This helps us to avoid overbooking to the point that our clinic becomes behind.”
Consider creating a call center. “We developed a centralized scheduling department for our 9 offices,” said Ms. Fridl. “These employees schedule all the appointments, triage phone calls, call in prescription refills, and direct all phone calls throughout the practice. We also developed an internal system to identify who is on hold for which office and how long they have been on hold so each employee can respond to these calls in an efficient manner—all of these changes contribute to decreased patient wait times.”
|
Assess Performance Regularly
“What gets measured gets managed,” said Mr. Suneja. “Value-based payments are inevitable, so practices must make sure that patient satisfaction scores are good. Not only is this important in terms of compensation but it also reduces complaints from unhappy patients.” Dr. Han agreed, and added an easy rule of thumb for assessing wait-time performance: “We look at how long the last patient is discharged after their appointment. For instance, if our last morning clinic appointment is at 11:30 a.m., and the patient is discharged by noon, we have had a successful clinical session. Conversely, if the last patient is not discharged until 1:00 p.m., we have not, and we need to find the cause and make adjustments.”
___________________________
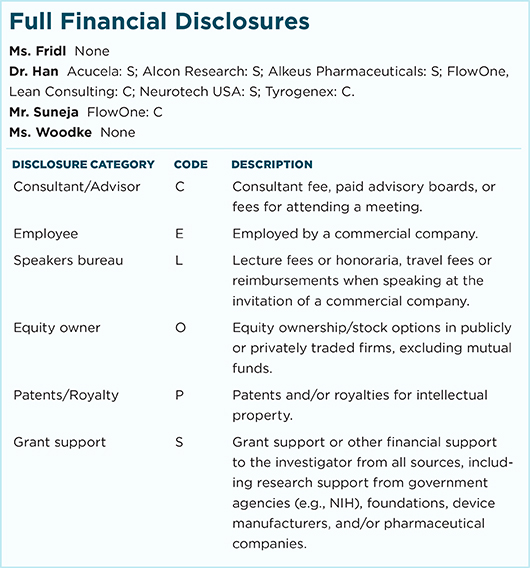
Ms. Fridl is chief performance officer at Asheville Eye Associates in Asheville, N.C. Relevant financial disclosures: None.
Dr. Han is director of the vitreoretinal service at the Medical College of Wisconsin in Milwaukee. Relevant financial disclosures: FlowOne: C.
Mr. Suneja is president of FlowOne Lean Consulting in Milwaukee, Wisc. Relevant financial disclosures: FlowOne: C.
Ms. Woodke is administrator at Oregon Eye Consultants in Eugene. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.