By Linda Roach, Contributing Writer, interviewing Robert A. Eden, MD, Omesh P. Gupta, MD, MBA, and Jonathan B. Rubenstein, MD
Download PDF
Fixation of posterior chamber intraocular lenses (IOLs) in eyes with inadequate capsular support remains a sticky problem in ophthalmology.
About 13 years ago, an Academy Ophthalmic Technology Assessment concluded that the available surgical approaches and IOL types for such eyes were equivalent in their visual and safety outcomes,1 a conclusion that held up in 2008, when the report was last reviewed for currency.
But the field of IOL fixation has not stood still since then. According to experts in complicated cataract surgeries, there has been a steady evolution in the techniques, devices, and materials for stabilizing IOLs in eyes with insufficient capsular support for posterior chamber implantation in the capsular bag or ciliary sulcus.
Spotlight on Suture Materials
Arguably, one of the most immediately significant developments relates to the material used for the fixation sutures. Concerned about late breakage of the 10-0 polypropylene sutures on which they had been relying, some surgeons began a few years ago to use an alternative with higher tensile strength: sutures made from expanded polytetrafluoroethylene (Gore-Tex), said Omesh P. Gupta, MD, MBA, at Wills Eye Hospital in Philadelphia.
“It is a very resilient suture, which is used for cardiac procedures such as valve replacement. And this underscores its resiliency because you wouldn’t want to sew a heart valve in with a suture material that has a breakage problem,” Dr. Gupta said.
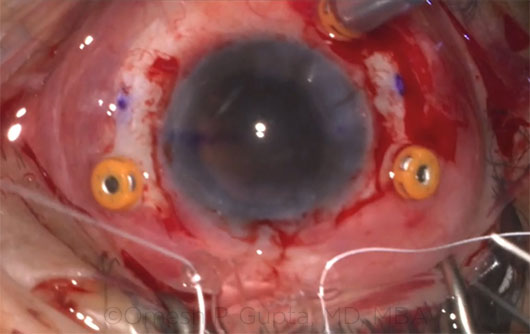 |
GORE-TEX. An Akreos lens is threaded with Gore-Tex sutures outside the eye (above). The temporal sutures are inserted through the wound and externalized through their corresponding sclerotomies. The lens is inserted. The nasal sutures are inserted and externalized, and the threads are tied, rotated, and buried. (For a short video, see below.)
|
The Polypropylene Story
There have been reports for more than a decade that 10-0 polypropylene fixation sutures (Prolene) were less durable in the eye than ophthalmologists had anticipated. One 2006 study reported that broken sutures occurred in 27.9% of the cases (n = 61), and the mean interval between fixation and breakage was 50 ± 28 months.2
The reports led to empirically based recommendations that if polypropylene is used to hold an IOL in place, the surgeon should use a thicker suture.3
The bottom line: “You should not use 10-0 Prolene at all. You should at least use 9-0 Prolene so you’ve got something that will be less likely to fail,” said Jonathan B. Rubenstein, MD, at Rush University Medical Center in Chicago.
A continuing problem of broken sutures. Even if 10-0 sutures were never used again, however, an unknown number of pseudophakes whose sutures were 10-0 might be presenting in future years with broken sutures and subluxated IOLs, Dr. Gupta said.
“In the last year, our service at Wills has seen perhaps 4 or 5 dislocations due to suture breakage, so they are still relatively rare. But this is already happening, and it’s going to be continuing,” Dr. Gupta said. “With the breakage rate reported at anywhere from 5% to 25%, we expect to be seeing more and more of these cases, especially if the patients are living longer.”
Why the broken sutures? Polypropylene is difficult to handle and easy to damage intraoperatively, Dr. Gupta said. “You tie it too tight or tug it the wrong way, and it can break. It’s very fragile,” he said.
It has been reported that factors such as sharp IOL edges can sever the 10-0 sutures.4 And damage to the optic or haptics also has been reported.5
Other Developments in IOL Suturing
Patients who require suturing of their IOLs are benefiting from the procedural and device developments of the last several years, Dr. Rubenstein said. “The original bad reputation that sutured IOLs had 10 or 15 years ago is now improved with these new techniques and materials.”
Fixation with fewer sutures. New surgical techniques can be used to anchor IOLs to the sclera while minimizing—and in some cases eliminating—sutures. These techniques generally rely on the construction of intrascleral tunnels into which the haptics are tucked.
Glue-assisted procedures. Fibrin glue continues to be explored as a way to hold haptics steady during the early postoperative healing period, but American surgeons have been slow to embrace the idea, said Dr. Eden, who has performed about 25 glue-assisted scleral fixation procedures since 2012. “Glue-assisted scleral fixation seems to continue to be a hot topic at national meetings. Aside from our practice, I have seen limited adoption of this technique by our local comprehensive ophthalmologists.”
Dr. Rubenstein added, “In experienced hands this is a good procedure, but it is difficult to learn. So, in the U.S., suture techniques prevail over the glue technique.”
Preferred fixation sites. Pseudophakes are living longer today than in the past, and surgeons must take longevity into account when deciding where to stabilize a subluxated or secondary IOL, Dr. Rubenstein said. An IOL held in the bag or in the sulcus with sutures might be preferable to iris fixation, especially in younger adults, because of risks for iris damage over the long term, he said.
An IOL with 4-point fixation. Unlike previously available IOLs intended for suture fixation, a newer IOL (Akreos AO60; Bausch + Lomb) is foldable and therefore does not require a 7-mm incision, Dr. Gupta said. Although designed for conventional in-the-bag implantation, the AO60 lends itself to scleral suturing through eyelets in the 4 haptic “feet,” he said.
|
The Rise of Gore-Tex
Dr. Gupta and Dr. Rubenstein said they now perform most of their IOL fixations with Gore-Tex CV-8 sutures (equivalent to about 7-0 gauge).
Advantages. Last year, Dr. Gupta and colleagues at Wills published a study in the British Journal of Ophthalmology investigating short-term safety and efficacy of Gore-Tex sutures.6 The authors noted that there have been no reports of Gore-Tex suture degradation in the ophthalmic or nonophthalmic literature. In their study of 85 eyes with Gore-Tex–fixated IOLs, they saw no suture-related adverse events, including suture erosion/breakage and persistent postoperative inflammation, at a mean follow-up of 325 days. They listed the material’s advantages as “high tensile strength, high visibility due to its white colour, minimal inflammatory response and minimal memory, which makes it exceptionally easy to manipulate.”
Added Dr. Gupta: “My heart rate is a lot lower when I use Gore-Tex than it is with Prolene. It’s almost impossible to break a Gore-Tex suture. And you can make as small as a 27-gauge wound and still bury the knot in the sclera through it.”
Disadvantages. In contrast, Dr. Rubenstein said the major disadvantage of Gore-Tex is its thickness, which can make the suture knot harder to bury in the sclera. “I have found that it is difficult to bury in anything smaller than a 23-gauge hole. Also, the needle that comes swedged onto the Gore-Tex is not as sharp as the CTC-6, PC-7, or CIF-4 needles that are available on 9-0 Prolene,” he said. “That is why I prefer to either pass the Gore-Tex needle into a 25-gauge needle as a passer or cut off the Gore-Tex needle and grab the suture ab externo with a 25-gauge microforceps and pull it out of the eye through a 23- or 25-gauge scleral opening,” he said.
Which patient, which material? While Dr. Gupta prefers Gore-Tex for all IOL fixations, Dr. Rubenstein said he approaches the decision situationally.
“When the patient in a fixation case is younger than 60, I will use Gore-Tex almost all the time,” Dr. Rubenstein said. “When they’re older than 60, I will sometimes use Gore-Tex and sometimes use 9-0 Prolene, depending on the situation.”
Furthermore, he still uses polypropylene when suturing a 3-piece IOL to the iris. “If you do suture to the iris, there you can actually use either 10-0 or 9-0 Prolene—both those materials are acceptable,” Dr. Rubenstein said.
Off label: an impediment? Ophthalmologists have been slow to add Gore-Tex sutures to their procedural protocols, but usage appears to be creeping upward, Dr. Gupta said.
For instance, at Albany Medical College in Albany, N.Y., anterior segment surgeon and assistant professor Robert A. Eden, MD, said he switched to 9-0 polypropylene several years ago. This remains his first choice in suture material because “I was trained using Prolene,” Dr. Eden said, but he recently began his first Gore-Tex suture trials.
Dr. Gupta attributes the limited adoption of Gore-Tex to 2 factors. “First, Gore-Tex in the eye is relatively new. It’s only been described in the last several years, and it’s still catching on. Second, it’s not approved for use in the eye. This is an off-label use,” he said.
Dr. Rubenstein said he reassures cautious colleagues that they can be “totally comfortable” using Gore-Tex in this way. “Yes, it’s an off-label use, but there are many things that we ophthalmologists use that are off label,” he said. “When we treat a corneal ulcer with topical antibiotics, that’s off label as well, because these antibiotics actually were approved for conjunctivitis. I’m using the Gore-Tex because it’s necessary and in the patient’s best interests to do so.”
___________________________
1 Wagoner MD et al. Ophthalmology. 2003;110(4):840-859.
2 Vote BJ et al. Am J Ophthalmol. 2006;141(2):308-312.
3 McAllister AS, Hirst LW. J Cataract Refract Surg. 2011;37(7):1263-1269.
4 Parekh P et al. Ophthalmology. 2007;114(2):232-237.
5 Tanaka H et al. Case Rep Ophthalmol. 2014;5(2):212-216.
6 Khan MA et al. Br J Ophthalmol. Published online Aug. 28, 2015.
___________________________
Dr. Eden is a cornea and anterior segment surgeon and an assistant professor of ophthalmology at Albany Medical College, in Albany, N.Y. Relevant financial disclosures: None.
Dr. Gupta is a surgeon in the retina service at Wills Eye Hospital and an assistant professor of ophthalmology at Thomas Jefferson University Hospital, in Philadelphia. Relevant financial disclosures: None.
Dr. Rubenstein is a cornea and anterior segment surgeon, Deutsch Family Professor, and vice chairman of ophthalmology at Rush University Medical Center, in Chicago. Relevant financial disclosures: None.
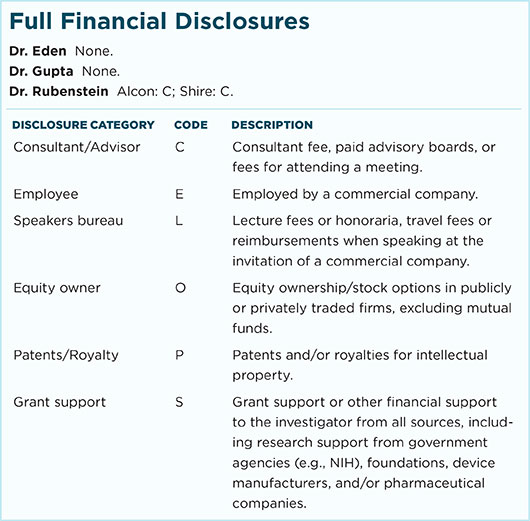
For full disclosures and the disclosure key, see below.