Download PDF
One of the biggest challenges with irregular astigmatism is simply thinking of it in the first place,” said William J. Dupps Jr., MD, PhD, at Cole Eye Institute in Cleveland. “You need to have it on your checklist of things to consider when a patient’s vision is either reduced or subjectively distorted in some way.”
Fairly uncommon, clinically relevant irregular astigmatism produces a curvature at each meridian that is not uniform. “Irregular astigmatism is not correctable with standard spectacles or contacts, but the degree of vision loss varies by how irregular and high the astigmatism is,” said Michael W. Belin, MD, at the University of Arizona College of Medicine in Tucson.
Causes of Irregular Astigmatism
Irregular astigmatism may be innate or acquired, said Christina R. Prescott, MD, PhD, at NYU Langone Health in New York City. Innate astigmatism is usually due to congenital corneal pathology that can either be stable or progressive, and acquired astigmatism is most commonly secondary to scarring or ectasia, she said. “You first want to determine the etiology and then figure out if it is stable or progressing. If it’s stable, you can treat it, but if it’s progressing such as from ectasia, you must first stop the progression.”
Corneal ectasia. Causing bulging and thinning of the cornea, ectasia is one of the most common causes of irregular astigmatism that Jack Parker, MD, PhD, sees in his cornea practice in Birmingham, Alabama. Keratoconus is the most common ectasia, but keratoglobus, pellucid marginal degeneration, and Terrien marginal degeneration also are characterized by irregular astigmatism, said Deborah S. Jacobs, MD, at Harvard Medical School in Boston.
Two more conditions. Two other common conditions may lead to irregular astigmatism, said Dr. Jacobs. These are Salzmann nodular degeneration, which is seen anterior to Bowman layer, and pterygium. Other less common corneal dystrophies and degenerations can also cause irregular astigmatism, she added.
Corneal scarring or surgery. Corneal lacerations or infections such as shingles or herpes simplex may cause scarring that leads to irregular astigmatism, said Dr. Jacobs, adding that it is also possible to acquire it from eye surgery that requires incisions at or near the corneal limbus. “This is less common with good surgical technique, but more likely when using larger incisions, or incisions near the visual axis,” she said. “It is quite common after a full-thickness corneal transplant, but much less common with endothelial keratoplasty. We’ve also gotten better at screening and modifying ablation profiles to avoid post-LASIK ectasia.”
Suspecting and Diagnosing Corneal Irregularity
“To find irregular astigmatism, you first have to suspect it because you can’t fully correct it with ordinary refraction,” said Dr. Jacobs. “Attempts at refraction may or may not get the patient close to 20/20, and sometimes the remaining deficit is attributed to something else, such as corneal scarring or macular issues.”
To get the correct diagnosis, the refractive evaluation should be thorough with pinhole testing and retinoscopy. “If you can’t achieve your pinhole, then it’s time to suspect irregular astigmatism,” she said. And by revealing an unusual red reflex, said Dr. Parker, retinoscopy can also be surprisingly helpful.
Review records—and listen. Always ask to review the patient’s records, if available, said Dr. Prescott. “Prior tomographic or topographic imaging is the most helpful, but even old glasses prescriptions or notes that include manual keratometry or other refractive measurements may be helpful as well.”
Dr. Dupps listens closely to the patient’s description of a visual complaint. “It’s amazing how often the patient will lead you to think about irregularity,” he said, advising to also ask about vision in ambient light conditions and what the patient sees when looking at a point of light. “If they describe a ghost image around the light or a streak of light in a certain orientation, that may be an indication of irregular astigmatism.”
Trial of rigid lenses. “Although it is somewhat of a lost art,” said Dr. Belin, the single best technique to diagnose irregular astigmatism and determine its clinical significance is trial of a rigid contact lens. “If the vision loss is secondary to irregular astigmatism, the rigid lens will correct it by creating a new optical surface on the cornea. By contrast, a soft lens tends to mold to the shape of the cornea, so it masks some but not all of the irregular astigmatism.”
Placing a rigid gas permeable corneal lens or scleral lens on the eye and refracting over it will eliminate any irregular astigmatism from the front of the cornea, added Dr. Jacobs, clarifying that posterior irregular astigmatism may exist but is usually minor.
It helps to explain to the patient why the lens trial might be worthwhile, said Dr. Dupps. “Most patients think it changes the shape of the cornea, so I explain that it’s simply sitting on the front of the cornea, optically neutralizing the irregularities.”
Beware opacities. Dr. Jacobs cautions against automatically attributing vision loss to opacities from infections, diseases, surgery, or injuries—rather than to the irregular astigmatism the scarring itself causes. “Do not operate for a scar without doing a rigid lens over-refraction first,” she emphasized. “You may find that the patient is fully or sufficiently correctable with lenses alone.” Moreover, a misdiagnosis may lead to unnecessary full-thickness transplants.
Imaging. Topography such as Placido disc-based devices (Bausch + Lomb Orbscan, Zeiss Atlas, and Nidek OPD-Scan) uses 2D curvature analysis. And tomography, typically Scheimpflug technology (Oculus Pentacam, Ziemer Galilei, or CSO Sirius), produces a 3D reconstruction of the entire cornea. “Either of these technologies, both by visual inspection of the curvature and/or an elevation map, can help you diagnose irregular astigmatism,” said Dr. Belin, “and they will also plot out the principal meridians. Nonorthogonal meridians are a hallmark of irregular astigmatism.”
With Placido disc-based devices, which involve a reflective system, distortion may make it impossible to analyze the surface information, Dr. Belin said. “The lack of information is at least a red flag that you may be seeing irregular astigmatism.”
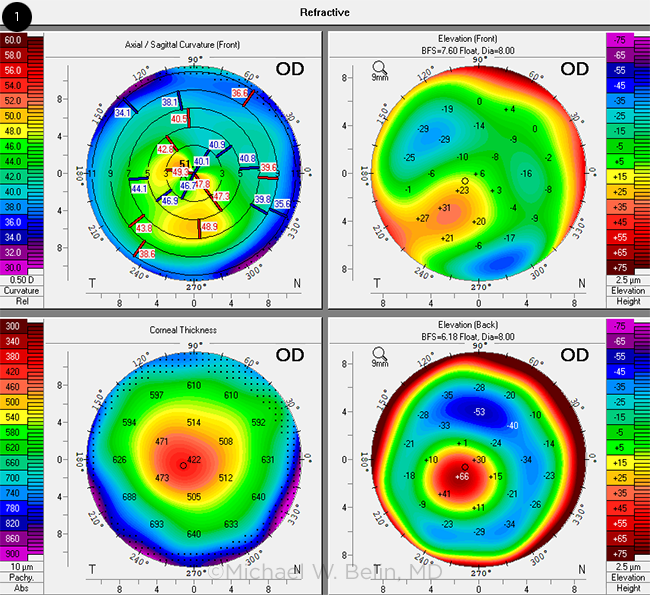
The gold standard, said Dr. Prescott, is the Pentacam (Fig. 1) or a similar tomography device. “Depending upon how worried I am about progression, I will ask the patient to come back in three- or six-month intervals, to repeat my imaging and exam.”
Screening surgical candidates. “We’ve gotten really good about using imaging for screening,” said Dr. Prescott, “so we find those patients with keratoconus and high astigmatism who are not good candidates for refractive surgery.” Dr. Dupps performs tomography as part of every cataract or refractive surgery evaluation. “We’ve come to understand how important it is to spot corneal irregularities before putting in a premium lens and expecting a good outcome,” he said.
Special considerations for children. Dr. Prescott underscored the importance of closely monitoring children with keratoconus and irregular astigmatism. Keratoconus is much more aggressive in children and can progress quite quickly, she said, “but if you catch it early and cross-link these children, you can dramatically reduce the need for corneal transplantation and the associated lifelong risk of ocular complications.”
 |
|
OCULUS PENTACAM. Refractive display of a patient with mild keratoconus. The upper left map (anterior curvature) shows nonorthogonal principal meridians, which is a hallmark of irregular astigmatism. The upper right (anterior elevation) and lower right (posterior elevation) show the classic positive island of elevation. The corneal thickness map (lower left) shows a moderately thinned cornea.
|
Specialty Contacts and CXL
“About 20 years ago, if a patient with irregularity from keratoconus couldn’t tolerate contact lenses, the only option was a full-thickness corneal transplant,” said Dr. Belin. “Now we have a number of different modalities, including specialty contact lenses.” This specialty lens repertoire, including soft and rigid corneal lenses in keratoconus designs, hybrid lenses, and scleral lenses, often offers full correction, added Dr. Jacobs.1
Things to consider. “If irregular astigmatism is present in only one eye, a specialty contact lens may not be the best option because the brain doesn’t do well with the sensations it receives from a single lens,” said Dr. Jacobs. “But if irregular astigmatism is present in both eyes or the patient is unsatisfied with his or her vision, specialty lenses should be offered.”
The biggest challenge is finding someone who knows how to fit a rigid or scleral lens, said Dr. Belin, adding that ophthalmologists should refer patients to a specialty lens fitter if their practice doesn’t include this service. “The patient needs to work with someone who is adept at fitting lenses because these are not standard fittings,” he said. “Equally difficult is getting the patient to learn how to handle and tolerate the lenses.”
Scleral and gas permeable lenses. Scleral lenses, large contact lenses that rest on the sclera, have emerged in the last decade as being easier to fit than rigid corneal lenses, said Dr. Jacobs. “They are now often the go-to choice for specialty lens fitters.”
Many patients can’t tolerate rigid gas permeable lenses, but they may do well with scleral lenses, said Dr. Prescott. “Corneas that are very irregular probably need a full scleral lens,” she said, “while others may do well with a miniscleral lens, which is smaller and may be more comfortable.” Another benefit of scleral lenses? “The saline solution [reservoir between the lens and cornea] can be therapeutic for [a patient with] ocular surface disease, which is associated with many ectasias,” she said.
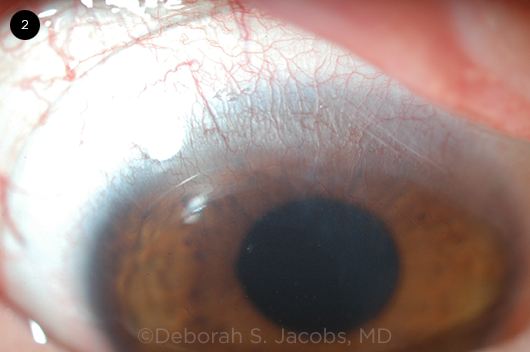
Custom lenses. The PROSE (Prosthetic Replacement of the Ocular Surface Ecosystem, Fig. 2) device is a highly customized scleral lens. It was developed at BostonSight, where Dr. Jacobs was employed in the past. “The fitter uses CAD/CAM software to modify the shape of the lens, which comes in diameters larger than are typical for commercially available scleral lenses,” she said. “Since PROSE was developed, the company launched a less custom version, which is more widely available, is ordered as any scleral lens would be, and is less expensive.”
Another way to make a highly custom scleral lens, she said, is by taking a mold and using computer software to design and print a lens off that base. Called the EyePrintPRO (EyePrint Prosthetics), this lens closely matches the unique scleral contours of a patient’s eye.
Other lenses. Other types of lenses may correct certain amounts of irregular astigmatism. There are commercially available soft lenses and rigid corneal lenses in special keratoconus designs. Hybrid lenses are rigid gas permeable in the center with a skirt of soft lens material, said Dr. Jacobs. And for those who can’t tolerate corneal rigid lenses, a piggyback system puts the rigid lens over a soft lens.
How to choose. Although the best specialty lens fitters will have all these lenses in their repertoire, said Dr. Jacobs, the clinical decision is based on the contours of the cornea, the relationship of the lid to the globe, and the patient’s lens-handling capabilities. “My experience has been that a well-fit scleral lens gives the most satisfactory result, especially for eyes with highly irregular or very high astigmatism.”
Cross-linking. In patients with keratoconus, corneal cross-linking (CXL) is another option. It strengthens and flattens the cornea, halting progression of the disease and also typically reducing the amount of irregular astigmatism, said Dr. Belin. “In the United States its use is largely limited to patients with progressive disease, which insurance companies cover.” He noted that he hopes the new ABCD keratoconus classification system2 will allow intervention at a much earlier period.
Epi-off versus epi-on. In the United States, the only FDA-approved CXL modality is epi-off CXL, which involves removal of the epithelium before applying riboflavin. “The epi-on technique is likely to be safer by causing less infection and persistent epithelial defects,” said Dr. Dupps, “but a significant percentage of these patients end up sloughing their epithelium, and the amount of corneal flattening seen with epi-off is greater than with epi-on due to enhanced stiffening.” A large clinical trial with many U.S. groups participating is currently evaluating the effectiveness and safety of epi-on CXL for keratoconus patients, said Dr. Prescott.
In 2011, Dr. Dupps and Abhijit Sinha Roy published a concept paper, demonstrating a more targeted approach to CXL3 that is now in clinical trials. “Instead of cross-linking across the whole cornea, which prevents part of the cornea from responding,” said Dr. Dupps, “you treat the weakest part, making it stiffer again so the whole cornea can bend back into a more normal configuration.”
 |
|
SCLERAL LENS. A PROSE scleral lens in a patient with limbal fibrosis and irregular astigmatism from Stevens-Johnson syndrome.
|
Remodeling and Refractive Surgeries
Intacs. Implantable intracorneal ring segments, Intacs (Addition Technology) are two small arcs of PMMA placed deep in the cornea to support and flatten the corneal topography. Dr. Dupps uses this corneal remodeling technique frequently for keratoconus patients; occasionally, he uses it for patients with postkeratoplasty irregular astigmatism.
“These do have a role for keratoconus,” said Dr. Jacobs, “but they can be a little unpredictable or disappointing—giving less sharp vision than a rigid contact lens.” Dr. Prescott has not used them, but she treated a patient whose Intacs actually extruded, causing scarring and neovascularization. This migration problem may occur due to an inflammatory response or an eye-rubbing habit, which is common in patients with keratoconus, said Dr. Dupps. He added that the good news is that Intacs can be removed, if necessary.
CAIRS. Similar to Intacs is a newer remodeling procedure called corneal allogenic intrastromal ring segments (CAIRS). “Instead of using PMMA, you use little strips of donor cornea, which confer some advantages,” said Dr. Parker. “They’re less likely to melt or to extrude, you get less glare or halos, and you can place them in much more severely aberrated corneas.” His practice has been using these as an alternative to Intacs, he said.
Pinhole pupilloplasty. “Many patients with highly aberrated eyes and severely warped corneas will see well if you provide them with a pinhole aperture,” said Dr. Parker. First described by Amar Agarwal, MD, pinhole pupilloplasty is a procedure that involves suturing the iris into a small pinhole, which has the effect of focusing light to provide a crisp image and an extended depth of focus, even with highly aberrated corneas, Dr. Parker said. “This is another option that’s been very useful for us in surgically treating irregular astigmatism.” However, rather than going straight to surgery, Dr. Dupps recommends a trial with pilocarpine drops first to simulate the results of a pinhole pupilloplasty.
IC-8 IOL. Approved by the FDA in December 2021, the AcuFocus IC-8 IOL creates a pinhole aperture at the center of the optic.4,5 Dr. Prescott said that she is looking forward to the prospect of using this lens in patients with irregular astigmatism who need cataract surgery. However, Dr. Jacobs questions the device’s widespread utility. “I think the limitations created by the small aperture will likely outweigh the benefits of any refractive correction achieved, making them impractical for most patients.”
LASIK with WaveLight Contoura. Alcon’s topography-guided laser ablation protocol, WaveLight Contoura, was recently approved for “normal” corneas but is currently also being used on irregular corneas. It precisely measures the cornea’s unique peaks and valleys and normalizes the shape of the cornea.6 “I wouldn’t use this approach for cases of keratoconus or other types of ectasia,” said Dr. Prescott, “but I would consider it for corneal scars or other stable causes of irregular astigmatism.”
___________________________
1 Jacobs DS et al. Cont Lens Anterior Eye. 2021;44(2):289-329.
2 Belin MW et al. Indian J Ophthalmol. 2020;68(12):2831-2834.
3 Roy AS, Dupps Jr. WJ. Invest Ophthalmol Vis Sci. 2011;52(12):9174-9187.
4 https://www.healio.com/news/ophthalmology/20211207/acufocus-receives-approvable-letter-from-fda-for-ic8-iol.
5 Langer J et al. J Refract Surg. 2021;37(5):312-317.
6 Motwani M. Clin Ophthalmol. 2022;16:111-126.
Meet the Experts
Michael W. Belin, MD Professor of ophthalmology and vision science, University of Arizona College of Medicine, Tucson, Ariz. Relevant financial disclosures: CXLO: C,O; Oculus: C.
William J. Dupps Jr., MD, PhD Refractive surgeon and cornea specialist, Cole Eye Institute and Cleveland Clinic Lerner Research Institute and professor of biomedical engineering, Case Western Reserve University, Cleveland. Relevant financial disclosures: Alcon: C; Cleveland Innovations: P; Glaukos: C.
Deborah S. Jacobs, MD Director of the Ocular Surface Imaging Center and associate professor of ophthalmology, Harvard Medical School, Boston. Relevant financial disclosures: None.
Jack Parker, MD, PhD Cornea specialist at Parker Cornea in Birmingham, Ala. Relevant financial disclosures: None.
Christina R. Prescott, MD, PhD Director of cornea services, vice chair for education, and associate professor of ophthalmology, NYU Langone Health, New York. Relevant financial disclosures: None.
Full Financial Disclosures
Michael W. Belin, MD CXLO: C,O; Oculus: C.
William J. Dupps, Jr., MD, PhD Alcon: C; Cleveland Clinic Innovations: P; Glaukos: C; National Eye Institute: S.
Deborah S. Jacobs, MD Simple Contacts: C,O; TecLens: C,O; Cloudbreak Pharma: C; Dompé U.S.: C; UpToDate: P.
Jack Parker, MD, PhD Eyevance: C; Glaukos: C.
Christina R. Prescott, MD, PhD Johnson & Johnson Vision: C; Santen: C.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Hired to work for compensation or received a W2 from a company. |
| Employee, executive role |
EE |
Hired to work in an executive role for compensation or received a W2 from a company. |
| Owner of company |
EO |
Ownership or controlling interest in a company, other than stock. |
| Independent contractor |
I |
Contracted work, including contracted research. |
| Lecture fees/Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Patents/Royalty |
P |
Beneficiary of patents and/or royalties for intellectual property. |
| Equity/Stock/Stock options holder, private corporation |
PS |
Equity ownership, stock and/or stock options in privately owned firms, excluding mutual funds. |
| Grant support |
S |
Grant support or other financial support from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and\or pharmaceutical companies. Research funding should be disclosed by the principal or named investigator even if your institution receives the grant and manages the funds. |
| Equity/Stock/Stock options holder, public corporation |
US |
Equity ownership, stock and/or stock options in publicly traded firms, excluding mutual funds. |
|