By James Wilhite, MD, Jeremy Maylath, and Kenneth C. Lao, MD
Edited By: Ingrid U. Scott, MD, MPH
Download PDF
Yasmeen Yodel,* a 24-year-old Black schoolteacher, had been struggling to read and grade test papers because of a rapid decline in her vision. Over the past five days, her surroundings seemed to appear progressively more dim. By the time she came to our clinic, she could no longer see out of her right eye. Similar visual loss was occurring in her left eye, but she could still see figures. In addition, her eyes hurt a little when she looked around. She also mentioned having a vague global headache and bilateral thigh soreness, which started around the same time as her eye problems.
She initially thought that this would resolve, as she had a prior episode of vision loss in her right eye about 10 to 15 years earlier after being hit in the head with a volleyball. That time she had been placed on IV steroids, as she recalled, and her vision returned to normal. This time, her vision loss was much worse.
Presentation
History. Ms. Yodel told us that she had not experienced recent weight gain, transient visual obscurations, pulse-synchronous tinnitus, or focal neurologic symptoms such as weakness, numbness, or tingling in the extremities or the face. She had no history of recent travel, illnesses, fevers, or rashes. She was not taking medications and had no known medical problems.
Exam. When we initially examined Ms. Yodel, she had no light perception (NLP) in her right eye and hand-motion (HM) vision in the left eye. The pupillary exam was remarkable for a 6-mm nonreactive right pupil and a 6-mm left pupil that sluggishly constricted to 4 mm. She also had a 1+ relative afferent pupillary defect in her right eye by reverse. Her intraocular pressures and anterior segment exam were normal.
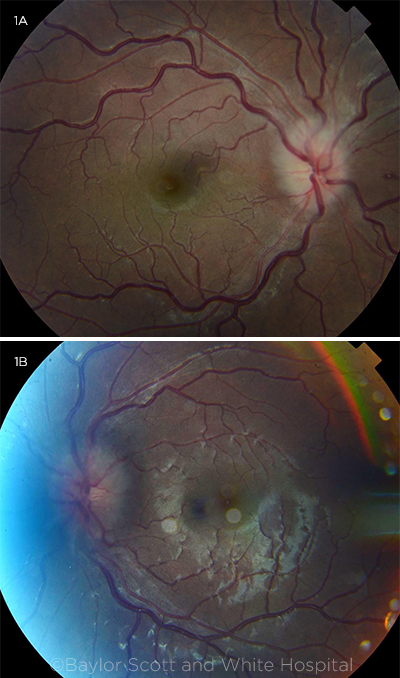
The dilated fundus exam revealed bilateral swollen optic nerves, with a flame hemorrhage nasal to the disc in the right eye and cotton-wool infarcts inferior to the disc in the left eye (Fig. 1). Vessels were mildly tortuous in both eyes. The macula was normal, and there were no anterior vitreous cells in either eye. Peripheral retinal exam was normal.
 |
|
FUNDUS BEFORE TREATMENT. Fundus photos show bilateral optic nerve head swelling and tortuosity of the vessels. There is a flame hemorrhage nasal to the optic nerve in the right eye and cotton-wool infarcts inferiorly in the left eye.
|
Differential Diagnosis
Clinically, Ms. Yodel presented with a bilateral optic neuropathy, which was likely optic neuritis, given her pain with eye movements. She had no symptoms of elevated intracranial pressure to suggest idiopathic intracranial hypertension and was not taking any medications or using any substances to suggest a toxic etiology. Her age would fit with a hereditary optic neuropathy, but we felt this was less likely than optic neuritis, given her pain with eye movements.
With the presumed diagnosis of a bilateral optic neuritis with severe vision loss, her presentation seemed most consistent with an inflammatory demyelinating optic neuritis, a category that includes neuromyelitis optica (NMO) and myelin oligodendrocyte glycoprotein immunoglobulin G (MOG-IgG)–associated optic neuritis. However, infectious and other autoimmune etiologies still had to be ruled out.
Next Steps
We admitted Ms. Yodel to the hospital and empirically started her on IV ster-oids (Solu-Medrol 1g/day) and consulted the neurologist, who started the patient on plasma exchange therapy. Upon admission, we ordered the following: magnetic resonance imaging (MRI) of the brain and orbit with and without contrast, magnetic resonance venography (MRV) of the head, lumbar puncture (LP) with opening pressure, cerebrospinal fluid (CSF) studies, and an extensive lab workup.
Early test results. These results were available within the first 24 hours:
- C reactive protein (CRP): 4.3 mg/L; erythrocyte sedimentation rate (ESR): 23 mm/hour
- Complete blood count (CBC) and comprehensive metabolic panel (CMP): within normal limits
- Antinuclear antibody (ANA): negative
- Antineutrophil cytoplasmic antibodies (ANCAs): negative
- Bartonella henselae and quintana: negative
- Rapid plasma reagin (RPR): negative
- Lyme antibodies: negative
- Meningitis/encephalitis panel: negative by polymerase chain reaction (PCR)
- LP opening pressure: 20 cm CSF
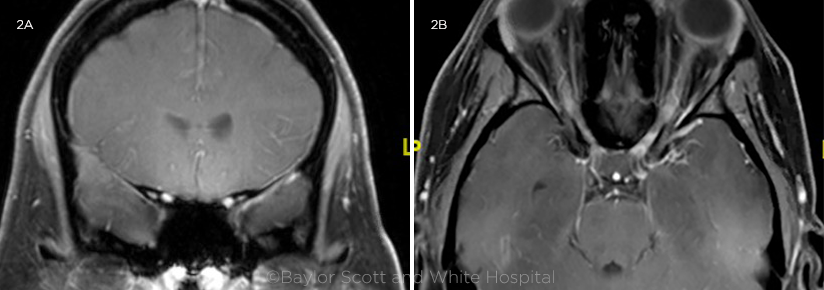
Imaging. On MRI, the patient’s brain appeared normal, without evidence of demyelinating lesions. However, extensive segments of both optic nerves showed enhancement (Fig. 2). MRV was unremarkable.
Results pending. The following tests were also performed, but the results took longer to become available:
- CSF studies
- Aquaporin-4 (AQP4) antibody
- MOG-IgG assay
 |
|
MRI. (2A) T1 coronal view, with fat suppression and contrast and (2B) T1 axial view with fat suppression and contrast; both show long segments of bilateral optic nerve enhancement. MRI of brain was normal, without any demyelinating lesions.
|
Clinical Course
Diagnosis. The day after starting therapy, Ms. Yodel’s eye pain, bilateral thigh soreness, and headache resolved. Three days later, her vision improved from NLP to HM in the right eye, and from HM to 20/20 in the left eye. After a few days, her MOG-IgG test result came back positive, confirming our suspicion of a demyelinating optic neuritis.
Our patient’s progress. She completed five days of IV steroids and was discharged home on a tapering regimen of oral steroids. Her oral steroids were tapered slowly over two to three months, and her neurologist started her on rituximab around six weeks after initial presentation.
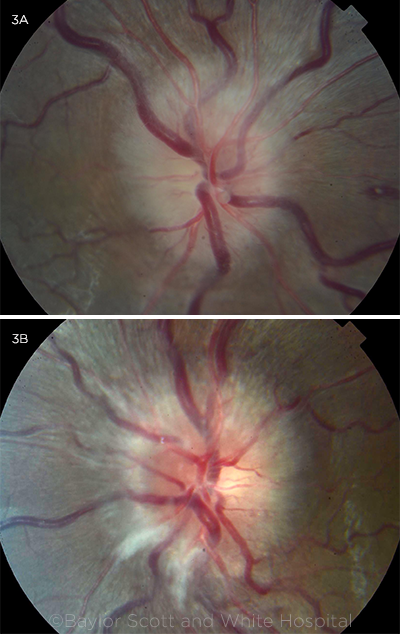
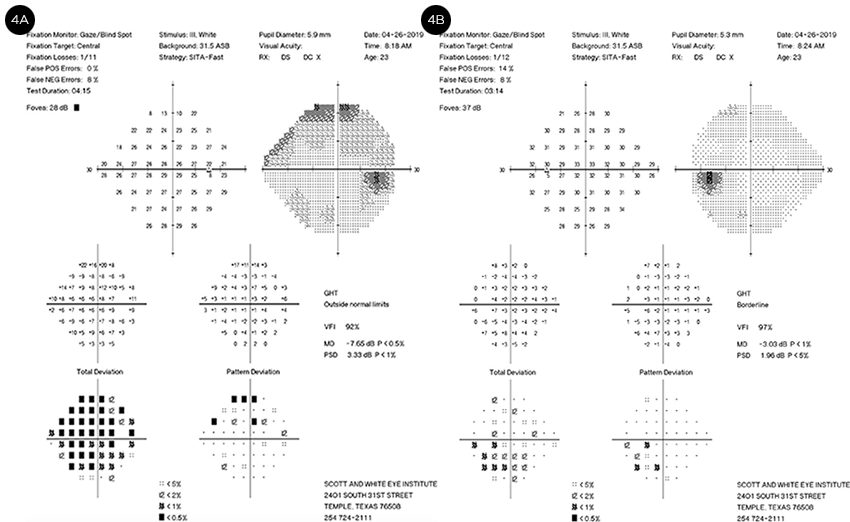
One month after initial presentation, Ms. Yodel’s vision had improved to 20/25 in the right eye and remained at 20/20 in the left. On Hardy-Rand- Rittler (HRR) color testing plates, she identified 0/6 with her right eye and 4/6 with the left; and her 1+ RAPD in the right eye was still present. Three months after her initial presentation, her vision was 20/20 in both eyes and HRR color plates were 2/6 in the right eye and 6/6 in the left, with persistence of the 1+ RAPD in the right eye. Fundus photos showed resolution of optic nerve head edema (Fig. 3). Visual fields were also improved at this time, although the right eye showed more significant residual deficits than the left (Fig. 4).
 |
|
AFTER TREATMENT. At three-month follow-up, optic nerve head swelling had resolved in both eyes, with temporal pallor of the disc more apparent in the right than the left eye.
|
Discussion
Myelin oligodendrocyte glycoprotein (MOG) is a surface protein located on oligodendrocytes in the optic nerve. Seropositive MOG-IgG optic neuritis has been established as a new subset of optic neuritis, with a growing number of cases published in the literature. It can present in a manner similar to NMO, with a recurrent course and profound vision loss, but is much more responsive to steroid therapy than is NMO.
MRI shows perineural or extensive longitudinal enhancement of the optic nerve in MOG-IgG (as seen in our patient, Fig. 2).1 Many patients who had been diagnosed in childhood with acute disseminated encephalomyelitis (ADEM), a rare inflammatory demyelinating disorder of the central nervous system, are now being found to be MOG-IgG positive.2
Chen and colleagues studied the characteristics of 87 patients with seropositive MOG-IgG optic neuritis who presented between 2001 and 2017.1 They found the following features:
- 57% were female.
- Median age was 31 years.
- Median number of optic neuritis attacks was three.
- 37% of patients had at least one attack with bilateral involvement.
- Average visual acuity (VA) during the worst attack was counting fingers, with final average VA of 20/30.
- Only 6% of patients had a final VA worse than 20/200 in either eye.
- Optic disc edema present in 86%.
- Pain with eye movements present in 86%.
- MRI findings: Perineural enhancement was seen in 50%, and 80% had extensive longitudinal involvement.
This case demonstrates many of the typical features of MOG-IgG optic neuritis: severe visual impairment, bilateral involvement, rapid visual improvement with steroids, possible recurrence, optic disc swelling, and long segments of optic nerve enhancement on MRI.
 |
|
VISUAL FIELDS. Improvement in visual field defects was seen at three-month follow-up, with more significant visual field defects remaining in the right eye, correlating with the greater pallor in that eye.
|
Conclusion
In summary, MOG-IgG–seropositive neuroinflammation is an entity distinct from multiple sclerosis and AQP4-IgG–seropositive NMO. Antibodies for MOG should be checked in patients with apparent optic neuritis when there is profound vision loss or lack of improvement in one month, as well as in bilateral cases, recurrent cases, or those with extensive or perineural enhancement on MRI.
Although there are no definitive guidelines for treating seropositive MOG-IgG optic neuritis, evidence suggests that these patients benefit from IV steroid pulse therapy, with or without plasmapheresis, for three to five days, followed by an oral steroid taper of longer duration than that recommended in the Optic Neuritis Treatment Trial. Steroid-sparing immunomodulatory agents should also be considered early in the course of disease to prevent relapses.
___________________________
1 Chen JJ et al. Am J Ophthalmol. 2018;195:8-15.
2 Huppke P et al. Mult Scler. 2013;19(7):941-946.
___________________________
*Patient name is fictitious.
___________________________
Dr. Wilhite is an ophthalmology resident, Mr. Maylath is a medical student, and Dr. Lao is a professor of neuro-ophthalmology; all are at the Baylor Scott and White Eye Institute in Temple, Texas. Financial disclosures: None.