This article is from March 2007 and may contain outdated material.
Last month, EyeNet began an exploration into a treatment for hemianopia called Vision Restoration Therapy, now being marketed by NovaVision. We closed with recognition by our interviewees that more studies are needed to determine its efficacy. This month we continue our conversations with those physicians.
One Treatment for Many Ills?
A particular mystery floating around VRT is the wide range of injuries for which the company says it works. Could insults from stroke, resections of tumors, apoptosis from inflammation and necrosis from trauma all respond to the exact same approach, as NovaVision suggests?
Persistent doubts. Very unlikely, said Jonathan C. Horton, MD. If NovaVision believes its therapy works for cerebrovascular accidents and motor vehicle accidents equally well, then the underlying rationale approaches the medically implausible, he said.
Dr. Horton is the author of one of a number of opinions on VRT published in the British Journal of Ophthalmology.1 In fact, his editorial addressed what would seem to be a physiologic impossibility behind VRT’s treatment of homonymous hemianopia: “The proposed mechanism for partial field recovery in patients with complete hemianopia was flawed. In such subjects the normal occipital lobe and the affected occipital lobe are physically separate—no fringe of injured but salvageable tissue exists that represents the border of the visual field. In this situation, why should visual rehabilitation therapy produce field recovery along the vertical meridian?”
Explicating the encephalon. But if visual recovery as proposed by VRT is improbable, then how do people who have had a stroke often recover the use of their extremities with therapy? Dr. Horton explained that injuries to the visual pathway, a sensory system with many contingent, serial components, cannot be easily compared with those involving motor functions, which can improve with repetitive, mechanical exercises. “With concerted effort, a hemiplegic patient can partially recover arm or leg control by exploiting muscle groups that still function. It is not clear that this analogy is suitable for the visual system. And in any case, the visual system, even an impaired one, is constantly getting stimulation during our waking hours, and it includes a very rich repertoire of motion, shapes and colors. There’s no basis to think that the artificial lights of perimetry will provide better stimulation.”
Recovery reconsidered. Bernhard A. Sabel, PhD, objected earlier to Dr. Horton’s point in a written opinion, arguing that neuroplasticity has been shown to be active in many regions of the brain, and not just those assigned to locomotion. “There is no reason why the visual system should be the great exception from all other functional systems of the brain,” he wrote.2 As for the seemingly broad applications for VRT, Jose G. Romano, MD, said that it is specifically designed to address damage that is static. In other words, the injury has happened and is finished; it is not progressive or inflammatory in nature. “In strokes, we tend to see damage that is discrete and limited. In trauma, it may be more scattered,” Dr. Romano said. “But the principle of plasticity is relevant in either case. There is no inherent reason to think it is not available throughout the brain. We see neuroplasticity in the motor cortex, the sensory cortex, the speech cortex and so on. So why wouldn’t we see it in the visual cortex? We are not suggesting that new neurons are created. Not at all. We think, though, that new synapses can be created to counter the deficit, much as we grow new synapses for everyday learning.”
The NovaVision board members we spoke to noted that the relative etiologies of brain injury, as different as stroke, tumors and trauma, were not crucial to the mechanism of VRT’s action. The brain, they explained, doesn’t care at the cellular level what happened. What matters is that latent connections between neurons adjacent to the damage can be called into use. These connections have been likened by advocates of neuroplasticity to roads that have not seen travelers in many years, but which suddenly become a convenient thoroughfare when nearby roads become impassable. Eventually, the new routing allows for recovered vision. They also described the principle of neuroplasticity as cell-based, not structure-based. As such, its potential should be conserved across most or all brain functions.
Although he believes neuroplasticity is conserved across the nervous system, Dr. Romano adds that he does not think its exact action is always uniform. He said many mechanisms of neuroplasticity have been suggested, including rewiring, reactivation of existing pathways, and the role of top-down attention function, in which the frontal lobes coach the occipital lobes along by telling them to “pay attention” to a task at hand.
 |
|
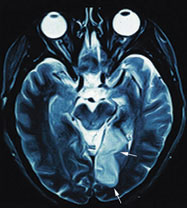
Postchiasmal Trouble. A right homonymous hemianopia resulted from this left parieto-occipital lob infarction.
|
What About Patient Perception?
Neuropathology arguments aside, there may be questions regarding the implications of claims on the NovaVision Web site.
Clearance vs. approval. NovaVision’s statement that VRT is “FDA-cleared” is technically correct, but it carries virtually no medical import, said Peter J. Savino, MD. To a hopeful patient who is not familiar with drug and device regulation, “FDA-cleared” might sound a lot like government approval. (Even a few of the physicians who advise NovaVision inadvertently used the word “approval” with us when discussing VRT.) But an FDA staffer explained that “clearance” only means the FDA views this device as roughly equivalent in risk and benefit to similar devices already on the market. Clearance is not the same as approval.
In fact, the FDA has two broad categories for evaluating medical devices. One is a relatively rigorous evaluation called a Premarket Approval (PMA) application, which must “include valid scientific evidence showing that the product does what it claims to do (is effective); and does not present unreasonable risks to the patient.”
NovaVision’s product, which no one describes as hazardous, easily fell into a second category of “lower-risk devices that require less rigorous testing and evaluation . . . Medical devices that go through the PMA process are called approved. Those that go through the 510(k) [less rigorous] process are called cleared.” (FDA’s emphasis.)
Everyone we spoke to at NovaVision pointed out, correctly, that the company had abided by the FDA’s own procedure for marketing a safe device.
Safety does not equal efficacy. But because VRT did not need the more rigorous evaluation, it was not tracked through methodical testing by interested physicians and researchers. That testing could have either verified or disproved VRT’s efficacy, and just as important would have brought it under the oversight of institutional review boards. As it is, Dr. Savino said, “Local IRBs aren’t involved because this device is not being marketed as experimental. It’s being offered as a service. If it was called experimental, patients couldn’t be charged for it.”
And charged they are. Patients desperate for some visual recovery are now paying around $6,000 for a course of VRT. The cost to patients is not mentioned on the NovaVision Web site, and neither is the fact that physicians offering VRT keep $3,000 of that.
Affiliation or advocacy? NovaVision lists 36 institutions—including some of the most prestigious eye centers in the country—where physicians who offer the treatment can be contacted. Misha L. Pless, MD, described that as evidence that the neuro-ophthalmology community sees the potential in VRT as a therapy for patients who have traditionally been given no hope for any recovery. But other physicians expressed concern that the names of leading eye centers, and, in some cases, even their logos, might resemble endorsements to impressionable patients.
Were patients satisfied,or just lucky? The Web site also says that more than 65 percent of VRT patients showed measurable improvements in their vision. Relative to this, it’s important to note that NovaVision has instituted a screening process to help physicians determine whether a particular patient is a good candidate for VRT.
This sounds reasonable, but some say it harbors the potential for “selecting for success.” That is, the screening may preferentially target patients who were more likely to improve even without treatment over patients who were randomly selected and less likely to improve. Dr. Savino noted that stroke patients, in particular, often recover substantial visual losses without any treatment.
 |
|
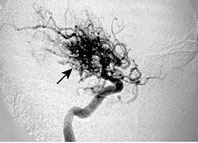
Postchiasmal Trouble. A left homonymous hemianopia was caused by this right basal ganglia arteriovenous malformation.
|
The Conversation Continues
Fresh trials, conducted by independent researchers with no financial ties to NovaVision, would clearly be welcomed by many in the neuro-ophthalmology community.
Two more editorials about VRT were published last December in Current Opinion in Ophthalmology.3 At the request of Robert C. Sergott, MD, professor and codirector of neuro-ophthalmology at Wills Eye Hospital, independent perspectives were submitted by Robert M. McFadzean, MD, and Christopher C. Glisson, DO. Dr. Sergott introduced the opinions by noting, “The debate has been intense, impassioned and public as to whether or not VRT is a tremendous breakthrough or poorly controlled clinical trial.”
For his part, Dr. Glisson suggested that patients’ subjective experience should not be arrogantly ignored: “Improvement in function should be regarded as the main goal of any treatment strategy, notwithstanding its effect on a single clinical test. With VRT, 80 percent of patients report improvement in activities of daily living, including visual confidence, reading, mobility and navigation.” But he added, “Until such a method [VRT] is validated by carefully controlled studies, subjective improvement in visual function stands alone as evidence of vision restoration therapy’s benefit.”
Dr. McFadzean contended that if VRT has true promise, then no one should fear proof through further investigation. “The medical advisors to NovaVision believe that VRT ‘results in visual improvement for certain patients with visual field defects.’ It is their professional duty to identify which patients and why, before further marketing of an expensive therapy to vulnerable, visually disabled patients.”
This story has legs (and hopefully axons). Assuming that neuroplasticity-based research has promise, both researchers and clinicians are eager to learn where in the visual system, and for which sorts of injuries, it would be expected to succeed.
What is certain now is that many well-intentioned and well-regarded physicians are wrestling with important questions of brain injury and vision recovery. Everyone shares the goal of making the world visible to patients living with darkness.
And for that, everyone needs a solution that can be held up to the light.
__________________________________
1 Horton, J. C. Br J Ophthalmol 2005;89:1–2.
2 Reinhard, J. et al. Br J Ophthalmol 2005;89: 30–35.
3 Sergott et al. Curr Opin Ophthalmol 2006;17:497–508.
__________________________________
Dr. Horton reports no related financial interests. Drs. Pless and Romano were given option grants for serving on NovaVision’s scientific and medical advisory board, but report no other related interests. Dr. Savino reports no related interests.