By Laura B. Kaufman, interviewing James Chodosh, MD, MPH, Elisabeth J. Cohen, MD, and Christopher J. Rapuano, MD
Download PDF
A number of factors have renewed concerns about, and sparked greater interest in, herpes zoster (HZ) among ophthalmologists. These include changes in epidemiology and recent findings about systemic sequelae, as well as a new vaccine in the pipeline and a nascent clinical trial for the ocular form of the disease.
Growing Problem
For reasons that are not completely clear, the incidence of HZ in the United States and worldwide has been increasing. From 1992 to 2010, the rate rose 39%,1 and the Centers for Disease Control and Prevention (CDC) now estimates that half of Americans who live to age 85 will develop shingles.2 A 2011 study indicates that mean age of onset is 52, which the authors noted is younger than that found in previous studies.3
Systemic sequelae. Associations between zoster and several serious systemic sequelae are coming to light. It has long been known that zoster is a risk factor for potentially fatal stroke. This is particularly true for herpes zoster ophthalmicus (HZO), a 2016 Academy policy statement said.4 In support of this, a Neurology study found that within 1 year of diagnosis, HZO patients had a 4.5 times greater risk of stroke than controls.5
Other systemic associations are also being explored in population-based studies. “There is a risk of malignancy being diagnosed, though it’s hard to know if this is cause and effect,” said Christopher J. Rapuano, MD, at the Wills Eye Hospital in Philadelphia. Further, the Academy policy statement noted linkages with temporal arteritis, heart attack, and depression.4 James Chodosh, MD, MPH, at Harvard Medical School, said that clinical data registries, such as the Academy IRIS Registry and others, will help make data more robust. “These will help us learn whether the associations are real.”
Herpes zoster ophthalmicus. There are more than a million new cases of HZ in the United States yearly. Of these, about 20% result in HZO.4 Along with HZ, the number of HZO cases may be rising. What’s more, age of onset may be dropping.
A retrospective chart review at Massachusetts Eye and Ear showed that the number of patients presenting with acute HZO rose from 71 in the year 2007 to 195 in 2013—though the researchers had insufficient data to calculate incidence rate. During this same time frame, the mean age of those diagnosed with acute HZO dropped significantly, from 61.2 years to 55.8 years.6
Ocular symptoms. As most ophthalmologists know, HZO can produce serious ophthalmic sequelae, including inflammatory anterior and posterior segment disease, neurotrophic ocular surface disease, glaucoma, and eyelid issues—often recurrently. “It is definitely potentially blinding or visually debilitating,” said Dr. Rapuano. “In the eye, it can cause inflammation for decades.”
 |
|
HZO. For patients who have had herpes zoster ophthalmicus, the experts recommend at least annual follow-up visits for several years to check for signs of glaucoma and keratitis.
|
Meeting the Challenge
How does this changing picture affect clinicians? Increasing awareness among physicians of HZ—and of its younger onset—is critical.
Include HZ in the differential. “For one thing, you have to suspect zoster in patients who come in with a rash, and unilateral moderate to severe pain often precedes the rash. It can certainly be shingles. This was always true but is more common now. You can’t dismiss it out of hand—you have to have zoster in your head as a possibility,” said Dr. Rapuano.
Dr. Chodosh agreed that physicians must suspect zoster “even in younger people who come in with specific symptoms. They don’t have to be immune suppressed to get shingles in their 20s. Unless you think about it, you could miss it.”
Ophthalmic follow-up care needed. “Another important issue is follow-up care by ophthalmologists,” Dr. Chodosh added. “Patients with shingles can have subclinical keratitis and not be aware of it. It can progress and be a problem before they know it. They can also develop transient or prolonged increases in eye pressure leading to glaucoma. I would say that if a patient ever had ophthalmic shingles, they should at least have an annual exam of the optic nerve and cornea because of those 2 risks. I see patients at least twice a year for several years after shingles.”
Vaccination Reduces the Burden
Currently, the only way to reduce the risk of shingles is with the vaccine, Zostavax (Merck). “The vaccine decreases the risk of getting zoster by about 50%; additionally, symptoms were less severe in the 50% who got the disease,” Dr. Rapuano said. He added that the vaccine can help decrease potentially debilitating long-term pain from postherpetic neuralgia (PHN). Specifically, the risk of PHN is reduced by 67%, according to the CDC, which also notes that the vaccine’s protective effect lasts about 5 years.7
Despite the promise of reduced risk of shingles and its sequelae, there are obstacles to adoption of the vaccine, as well as mixed messages about lowering the recommended age of vaccination.
Obstacles to vaccine adoption. Elisabeth J. Cohen, MD, at the NYU School of Medicine and Langone Medical Center in New York City, said that although HZ is a common and very serious disease, “only 28% of people aged 60 and older have been vaccinated as of 2014, according to the CDC. It’s not a new statistic, but it’s tragic that it continues and that primary care and eye doctors are not strongly recommending that patients get this vaccine.” Several factors in poor uptake of the vaccine are as follows.
Misconceptions still prevail. The truth, said Dr. Cohen, is that “HZ is not a disease of the elderly—half of the cases occur under age 60. And more than 90% of those who get it are not immunocompromised.” She surmised that mistaken beliefs may persist because public health officials may simply give more emphasis to contagious diseases.
Seriousness is not understood. Primary care providers tend to see milder cases and may not realize the repercussions of severe disease. “Once physicians see a patient who has had severe HZ, or who developed severe complications, they understand the importance of vaccination. Seeing is believing,” said Dr. Rapuano.
Cost of the vaccine. For many patients, the cost—at approximately $200—accompanied by variable insurance coverage and often high copays, can be a roadblock to vaccination, said Dr. Rapuano. From a societal perspective, though, he pointed out, “Obviously, there are cost issues of vaccinating millions. But, certainly, there are cost issues of getting zoster, including medical costs, pain, and suffering.”
Mixed message about age. Although the CDC continues to recommend vaccination at 60, Zostavax is FDA approved for persons aged 50 and older, and, Dr. Cohen noted, more than half of insurance companies cover vaccination starting at age 50.
In addition, the Academy’s policy statement on herpes zoster vaccine concluded that current evidence supports use of the vaccine for those 50 and up. It noted that the vaccine is considered most efficacious in preventing zoster in this age group, that more people in the group have zoster than any other age group, and that the disease carries significant risk for ocular and neurologic morbidity unrelated to pain. It stated, “Ophthalmologists should advise their eligible patients aged 50 years and older to obtain this vaccination.”
Dr. Chodosh added that vaccination is ever more important, with age at vaccination being a significant issue. He said that he is “hopeful that the age for vaccination will move to 50.” Dr. Rapuano concurred. “I recommend it to my patients over 50, and I got my vaccine the month I turned 50,” he said.
Looking Ahead
Questions remain about the best management approach. For example, Dr. Chodosh asked, “Should patients with recurrent ocular inflammation after shingles be treated with corticosteroids and an antiviral [i.e., valacyclovir]? Would patients who have had significant keratitis benefit from [oral] antiviral prophylaxis, similar to herpetic eye disease? This will be addressed in the upcoming ZEDS study by Dr. Cohen.”
ZEDS study. Dr. Cohen is spearheading the new Zoster Eye Disease Study (ZEDS), funded by the National Eye Institute, which will investigate treatment of HZO with long-term, low-dose valacyclovir. “It’s a placebo-controlled, double-masked trial to see if 1 year of valacyclovir is better than a placebo. We have a lot of data that chronic active infection is associated with inflammation and complications in the eye, as well as, most likely, stroke, coronary artery disease, and postherpetic neuralgia.”
She noted that earlier research has shown that “there is strong evidence that a chronic antiviral may be beneficial. Herpes simplex outcomes have been significantly improved with adoption of chronic antiviral treatment. Herpes simplex and varicella-zoster [viruses] have important similarities. In our study, we have the potential to lead the way, with the primary goal to reduce eye complications, as well as postherpetic neuralgia,” she said.
“It’s an exciting study, with 60 centers in 28 states and more than 100 investigators. We anticipate starting enrollment this month. We hope to show that if people are maintained for a year on low-dose oral valacyclovir, we can reduce eye complications.”
New vaccine in the pipeline. Last September, the New England Journal of Medicine reported the phase 3 placebo-controlled trial results for a new zoster vaccine (Shingrix, GlaxoSmithKline). Two injections of the vaccine were administered 2 months apart to trial participants age 70 and older. The vaccine showed 89.8% efficacy at a mean of 3.7 years after injection.8 An earlier study of the vaccine conducted with patients aged 50 and older showed 92.7% efficacy, across all age groups, over a 3.2-year span.9 Pooled analysis from both studies showed 88.8% efficacy against PHN.8
It is noteworthy that the newer vaccine does not include live attenuated varicella-zoster virus but contains an antigen from the virus and an adjuvant to boost immune response.9 Thus, Shingrix may in the future be an option for immunocompromised individuals, in contrast to Zostavax.
Dr. Chodosh noted that “a more efficacious vaccine may encourage more use.” However, he and other physicians say that—with a wait of around a year for the new vaccine—eligible patients should go ahead and receive the currently available vaccine.
Key Messages
What do the experts most want other ophthalmologists to know?
Encourage vaccination. “First, get vaccinated if you are 50 or older and immunocompetent, and encourage your patients to do the same. It’s a disease really worth preventing in people age 50 and above,” Dr. Cohen said. “An ounce of prevention could save your life.”
Dr. Rapuano said that if more physicians recommended the vaccine, “I would hope it could truly impact the public health picture. Incidence could go down by 50% or more. It’s something safe you can do prophylactically to decrease risk.”
Intervene early, aggressively. Dr. Chodosh emphasized that a patient’s pain should be treated aggressively at the onset of symptoms. “They often suffer far more than they admit to—it affects every aspect of their lives. Leaving the shingles patient to simply live with their pain is not necessary or appropriate.”
Raise awareness of HZ. All 3 physicians stressed that the disease deserves much more attention than it gets. “It is a critical public health problem. In my Boston clinics and the ER, the fellows and residents are pretty experienced with identifying the disease. We see huge numbers of cases,” said Dr. Chodosh, who is concerned that HZ may be underrecognized elsewhere.
“I think the ZEDS study will help in unanticipated ways, by increasing awareness of the disease and how devastating it is. It’s essential that we get a handle on zoster eye disease,” said Dr. Chodosh.
___________________________
1 Hales CM et al. Ann Intern Med. 2013;159(11):739-745.
2 www.cdc.gov/shingles/about/prevention-treatment.html. Accessed April 16, 2017.
3 Hernandez PO et al. J Clin Virol. 2011;52(2011):344-348.
4 AAO Policy Statement: Recommendations for Herpes Zoster Vaccine for Patients 50 Years and Older. 2016. Accessed April 16, 2017.
5 Lin HC et al. Neurology. 2010;74(10):792-797.
6 Davies EC et al. Br J Ophthalmol. 2016;100(3):312-314.
7 www.cdc.gov/vaccines/vpd/shingles/public/index.html. Accessed April 16, 2017.
8 Cunningham AL et al. N Engl J Med. 2016;375(11):1019-1032.
9 Lal H et al. N Engl J Med. 2015;372(22):2087-2096.
___________________________
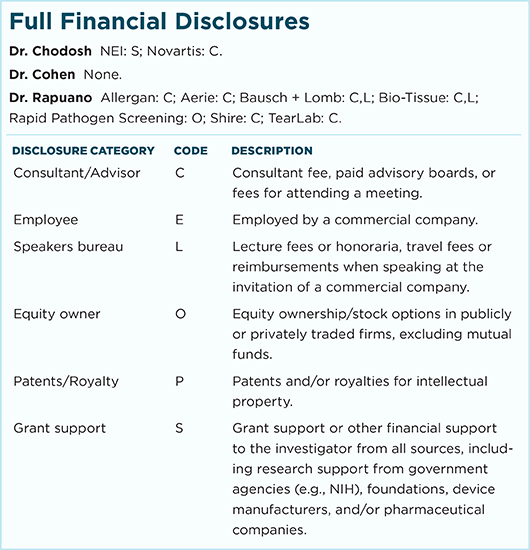
Dr. Chodosh is Cogan Professor of Ophthalmology at Harvard Medical School. Relevant financial disclosures: NEI: S.
Dr. Cohen is professor of ophthalmology at the NYU School of Medicine and Langone Medical Center in New York City. Relevant financial disclosures: None.
Dr. Rapuano is chief of the Wills Eye Hospital Cornea Service in Philadelphia. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.