By Leslie Burling-Phillips, interviewing Brad H. Feldman, MD, Lynn K. Gordon, MD, PhD, and Colin P. West, MD, PhD
Download PDF
Burnout is on the rise and has reached an alarming rate among physicians—approaching nearly 55% in 2014, which is an increase of almost 10% since 2011, according to a Mayo Clinic survey.1
Putting others first, self last. Improving the health of others is why most physicians attended medical school, but somewhere along the way, many physicians neglect their own wellness. “When we enter medical school, we are taught that we should place our patients’ needs above our own, so discussions about personal well-being often take a backseat to our professional responsibilities,” said Brad H. Feldman, MD.
One Physician’s Story: Never Enough Hours
Dr. Feldman became interested in physician wellness when he recognized early signs of burnout in himself and many of his peers. He was operating a busy private practice at Philadelphia Eye Associates, working as an attending at Wills Eye Hospital, directing a rapidly expanding academic global ophthalmology center, and serving as the Academy’s Secretary for Member Services, along with many other professional obligations. And at home, Dr. Feldman and his wife, who also works full time, were raising infant twins, which meant sleep was in short supply.
“Every minute of my life was accounted for, and I felt like there were not enough hours in the day to complete the ever-growing list of things that I wanted to do,” said Dr. Feldman. “I recognized that I was more easily agitated by stressors—sufficiently enough that my wife once laughed out loud when I snapped at her because she said she had never seen me get upset about anything. All of this made me interested in determining how to keep my life in balance, rather than being overcome by life’s stresses.”
Physician Wellness at AAO.org
This month, the Academy launches its newest online resource—Physician Wellness—at aao.org/wellness.
To help you nurture your well-being, this web page pinpoints the most useful tools and information, from handy apps to the peer-reviewed literature.
|
What About You?
Although ophthalmologists rank lower than their peers on the list of specialties reporting burnout, the numbers are still strikingly high at 43%. Watching for red flags and proactively addressing the common stressors will enable you and your practice to preempt the problem.
Common stressors. Ongoing drivers of stress include working long, inflexible hours; red tape; disruptive colleagues (see “Coping With a Toxic Colleague”); and, for too many surgeons, occupational injury.
Insufficient support. These stressors can be compounded by lack of support from organizational leadership, such as the department head or the practice’s managing physician, and a lack of understanding from friends and family, who may complain that your work life is eclipsing your personal life.
Stressors can fuel cognitive dissonance. The problem of cognitive dissonance “can occur when our career takes a different path from the expectations we had when we began medical training,” said Dr. Feldman. “This is often at the root of burnout.”
Recognize the red flags. Emotional exhaustion, depersonalization, and a sense of reduced personal accomplishment are all red flags for burnout. It can occur at any time in your career, and no one is immune, although some groups tend to be at an elevated risk.
Burnout can start early. Beginning ophthalmologists are confronted with unique stressors. When physicians start their first year of residency, they are often surprised because they hadn’t realized how difficult it can be to examine and treat the eye, said Dr. Feldman. “Initially, residency programs are very supportive and focus on resident skill and knowledge acquisition,” he said. However, “after a few months of hand holding, residents are expected to function as responsible members of the eye care team—at a time when many still doubt their abilities.”
Be aware of the imposter syndrome. Feelings of inadequacy—or the fear of being exposed as a “fraud”—can happen to anyone but are present in higher percentages of women and individuals from underrepresented groups in medicine, according to Lynn K. Gordon, MD, PhD. “There is evidence for an association between the imposter syndrome and higher levels of burnout.”2,3
Find a balance. “We understand that some of the personal approaches to burnout involve balancing one’s life and career—but this is often a challenge, particularly for those in a dual-career relationship, whether male or female,” said Dr. Gordon. “These are stressors that were not as prominent 50 years ago when there were fewer dual-career physician families.”
Understand the repercussions. On an organizational level, burnout can have major repercussions, leading to increased medical errors, reduced physician productivity, and a higher rate of physician turnover. On an individual level, this lack of wellness—if not addressed—can lead to broken relationships, alcohol and substance abuse, and/or depression and even suicide.1,4
Promoting Well-Being
Because everything in health care is under such financial scrutiny, organizations commonly ask whether they can spare the resources to support physician wellness—but is that the right question? “There is increasing evidence that not doing anything about the issue of burnout is costing the health care system an immense amount of money, and it should actually be a question of ‘how can we afford not to do something about this problem?’” said Colin P. West, MD, PhD, at the Mayo Clinic in Rochester, Minnesota.
Avoid the high cost of physician turnover. It is estimated that physician turnover in a practice could exceed $1M—or 3 times the salary and benefits package—per physician when the costs of replacing a physician (including recruiting and retraining a new physician) are factored into the equation, said Dr. West. By reducing turnover, investments in physician wellness can benefit your bottom line.
There is no one-size-fits-all solution. A common leadership mistake involves attempting to solve the problem of burnout from the top down by making broad and organization-wide changes, according to Dr. West, who described the importance of involving physicians in developing solutions: “By doing so, an organization develops a sense of community and partnership between the physicians and leaders.” This is critical because the problem is complicated, and the factors involved will likely differ between physicians and areas of practice, he said. “It is much more effective to look at the bigger picture and let the solutions present themselves by asking your team what they need, rather than creating a plan constructed around certain preconceived parameters—which work for some but will fail miserably for others.”
Small investments can have a large impact. Many effective interventions are relatively inexpensive and easy to implement, and they can result in tremendous improvements in physician well-being. For example, said Dr. Gordon, “creating networks to discuss common challenges and disappointments has been shown to decrease burnout and improve well-being. During these exchanges, individuals are able to recognize that others are facing similar challenges and share ideas about how to modify their own activities in order to reduce these stressors.”
Dr. West described the networking program introduced at Mayo Clinic in 2015: “As an institution, we want to foster connection and community. To support this philosophy, groups of physicians meet for lunch once or twice per month, for 6 months, to discuss topics common to the physician experience such as medical errors, generational differences in medicine, and work-life balance. The result is a demonstrated reduction in burnout, improvements in sense of community and togetherness, and overall improvements in markers for organizational health.” There was a $20 per meal allotment, so the investment was only about $240 per physician.
Abide by the 80/20 rule. “Engagement is the positive antithesis of burnout and is characterized by vigor, dedication, and absorption in work,” as researchers recently wrote.5 But how does one become engaged when both professional and personal stressors are ever-present?
The 80/20 rule refers to a simple tenet that can produce remarkable results: Spend at least 20% of your time participating in a professional activity that has the most meaning to you—whether it is teaching a course at the local community college, participating in academic research, or working with medical students, said Dr. West. “For many physicians, the most meaningful activity is direct patient care. A simple solution is often a matter of relieving physicians of clerical burdens so they are able to spend more face-to-face time with their patients, perhaps by hiring a scribe or reassigning responsibilities to other staff members.”
Take Care of Yourself
Determine what works best for you. What works for others may not work for you. “Be open, honest, and self-reflective, and examine your own personal needs and your family’s needs,” said Dr. Gordon. “Be open to change in order to regain equilibrium when necessary. There is no need to have your entire career plotted out in detail by age 30; make goals decade by decade according to what fits best at the time so that you will be a fulfilled physician who takes excellent care of your patients and yourself.”
What’s good for your patients is good for you. Applying the basic principles of health care that you advocate to your patients is the best place to start when thinking about personal wellness. “Even as ophthalmologists, many of us do not get our eyes regularly examined or take the time to see our primary physician. Exercising, maintaining a healthy diet, and sleeping well cannot be underestimated in terms of how important it is to feeling and performing well as a physician,” said Dr. Feldman.
___________________________
1 Shanafelt TD, et al. Mayo Clin Proc. 2015;90(12):1600-1613.
2 Legassie J et al. J Gen Intern Med 2008;23(7):1090-1094.
3 Villwock et al. J Med Educ. 2016;7:364-369.
4 Dyrbye, et al. National Academy of Medicine. (2017) Accessed Sept. 26, 2017.
5 Shanafelt TD, Noseworthy JH. Mayo Clin Proc. 2017;92(1):129-146.
___________________________
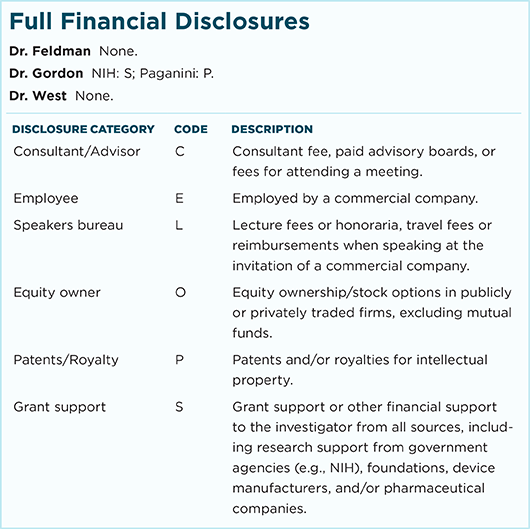
Dr. Feldman is at Philadelphia Eye Associates, Wills Eye Hospital. Relevant financial disclosures: None.
Dr. Gordon is senior associate dean for diversity at the David Geffen School of Medicine at UCLA. Relevant financial disclosures: None.
Dr. West is an internist at the Mayo Clinic in Rochester, Minnesota. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Wellness Events at AAO 2017
SUNDAY, NOV. 12
YO (Young Ophthalmologist) Program (event code Spe13). This features a 40-minute wellness segment:
- Get Up and Move—Ergonomics and Physician Wellness (Camille Palma, MD)
- Life Hacks—Succeed at Life and Focus on What Matters (Rob Melendez, MD, MBA, Brad Feldman, MD, and Janice Law, MD)
- Finances for an MD by an MD: Career Checklist (Mark Melson, MD). When: Sunday, Nov. 12, 1:10-1:50 p.m, during the YO Program (10:00 a.m.-2:00 p.m.). Where: Room 252. Access: Free.
Physician Wellness and Its Impact on Patient Safety (during Sym18). Presenter: Brad H. Feldman, MD. When: 3:50-3:55 p.m., during Unresolved Challenges in Patient Safety: Finding a Way Forward (Sym18; 3:15-5:30 p.m.). Where: Room 275. Access: Free.
MONDAY, NOV. 13
Physician Wellness (Sym24). Chairs: Lynn K. Gordon, MD, PhD, and Florentino E. Palmon, MD.
- What Is the State of Physician Well-Being? (Brad H. Feldman, MD)
- What Impacts Physician Well-Being (Cynthia Ann Bradford, MD)
- Physician Burnout: Prevalence, Drivers, Consequences, and Mitigating Strategies (Lotte Dyrbye, MD)
- Panel Discussion
- Stress and Mindfulness: Harnessing Them for Wellness (Michael D. Lumpkin, PhD)
When: 8:30-10:00 a.m. Where: La Nouvelle Orleans C. Access: Free.
Can We Have It All? Building and Balancing—Tools for Thriving at Career and Life (Sym31). Chairs: Purnima S. Patel, MD, and Jeff H. Pettey, MD.
- Approaches to Physician Wellness: How to Identify Symptoms and Measures to Take (Julia A. Rosdahl, MD, PhD)
- Balancing Career Building With Family Building: High-Yield Pearls to Growing Your Career (Tamara R. Fountain, MD)
- Seeking Opportunities as a YO While Dealing With an Illness in the Family (Janice C. Law, MD)
- Balance for Young Leaders: Going Through Burnout and Coming Out Ahead (Jeff H. Pettey, MD)
When: 10:15-11:45 a.m. Where: La Nouvelle Orleans C. Access: Free.
Burnout in Ophthalmology: Starting and Finishing (LL25). Presenters: Jean E. Ramsey, MD, MPH, Alfredo A. Sadun, MD, PhD, Frederick T. Fraunfelder, MD, and Oscar Alfredo Cruz, MD. When: 11:00 a.m.-noon. Where: Learning Lounge 1 (Hall G, Booth 3847). Access: Free.
Ergonomics/Musculoskeletal Disorders in Ophthalmologists (Spe22). Presenters: Jeffrey L. Marx, MD, Renee Ostertag, DDPT, MPT, and Scott E. Olitsky, MD. When: 12:45-1:45 p.m. Where: Room 242. Access: Free.
|