This article is from November/December 2010 and may contain outdated material.
Aspheric lens surfaces have become an attractive feature for new IOLs over the last decade, since ophthalmologists began applying the lessons learned from laser vision correction to cataract surgery. These lenses are designed to eliminate the positive spherical aberration added by traditional IOLs to the pseudophakic visual axis. But IOL makers took different roads to asphericity, yielding a collection of aspheric lenses that variously seek to neutralize all, some or none of the visual system’s naturally occurring corneal spherical aberration.
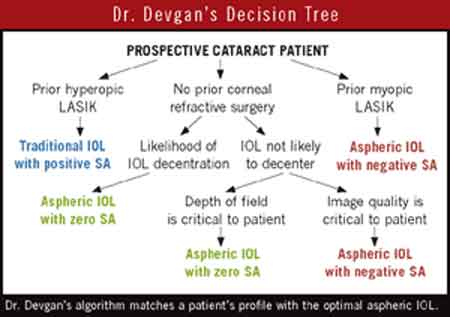
Consequently, today’s cataract surgeon should choose aspheric IOLs based on the characteristics of the individual patient’s eye, said Uday Devgan, MD, associate clinical professor of ophthalmology at the University of California, Los Angeles and chief of ophthalmology at the UCLA Medical Center. Dr. Devgan has developed a decision tree based on the premise that each aspheric IOL design offers potential benefits for certain patients (see “Dr. Devgan’s Decision Tree”). “There are benefits to each of the different aspheric IOL types. You just have to make choices based on the patient’s ocular characteristics,” Dr. Devgan said. “Surgeons have to be comfortable with all of the options.”
What will the average patient notice? Jay S. Pepose, MD, PhD, clinical professor of ophthalmology at Washington University in St. Louis, understands the desire to give patients the best possible postoperative vision and image contrast. But based upon the work by Wang and Koch,1 he is skeptical about the clinical impact of choosing a specific aspheric IOL to eliminate spherical aberration based upon measuring corneal spherical aberration alone. “Clearly we have reached the point where aspheric lenses are the standard,” Dr. Pepose said. “But the debate is over whether reducing the positive spherical aberration to zero is going to make much difference to the average cataract patient with mesopic pupils less than 5 mm. However, for a patient with large mesopic pupils who does a lot of night driving, there may be a distinct advantage to implanting an aspheric IOL that offsets the cornea’s positive spherical aberration, in an effort to maximize contrast sensitivity and minimize night myopia.”
The Options
The first negatively aspheric IOL on the market, the Tecnis Z9000 (Abbott Medical Optics), emerged from a decade of basic studies showing that the positive spherical aberration of the human visual system increases with age.2,3 The modified prolate anterior surface of the Tecnis was optimized to neutralize the average level of positive spherical aberration (+0.27 µm) found in an earlier research study.3,4
The aspheric IOLs now available in the United States are designed to neutralize only about half of the cornea’s positive aberration (AcrySof IQ by Alcon and iSymm by Hoya Surgical Optics). And other ophthalmic firms shape their aspheric IOL surfaces to have little to no impact on spherical aberration (Bausch + Lomb’s Crystalens AO, SofPort and Akreos AO; Staar Surgical’s Afinity and nanoFlex).
Studies generally have shown greater contrast sensitivity, particularly in dim light, and better performance on night-driving tests with Tecnis compared with spherical IOLs, and, in some cases, also compared with other aspherics.5,6 But lower spherical aberration reduces pseudophakic depth of field,7 and there has been concern about optical degradation if the IOL were to tilt or decenter.8
Prior refractive surgery? For a minority of cataract patients, the choice of IOL is critical because they already are hampered by high aberration from refractive surgery, both Drs. Devgan and Pepose noted. “If someone had hyperopic LASIK, they’ll have a lot of negative spherical aberration already. You don’t want to add to that and make their quality of vision worse,” said Dr. Pepose. In these patients, a traditional, spherical IOL can be used to offset the negative spherical aberration in their post-hyperopic LASIK eyes, he said. If the LASIK was for myopia, a negative spherical abberation IOL will give the patient optimal acuity.
More contention on refractive surgery- naïve patients. But the surgeons disagree about the value of using negative spherical abberation IOLs to neutralize corneal aberration in cataract patients who have not had refractive surgery. Dr. Devgan believes that the potential benefits of reducing spherical aberration are worth pursuing, even if the potential gain is small. Dr. Pepose doubts the clinical utility of doing so.
“There have been multiple studies in which patients with the same model of IOL, one aspheric and one not, have had a hard time seeing any difference in vision between their two eyes,” Dr. Devgan said. “The visual differences from reducing corneal spherical aberration are subtle but still an incremental improvement in vision.”
Are templates a good idea? Dr. Pepose noted that some researchers want to simplify the aspheric IOL choices by determining whether patients can be stratified by levels of corneal spherical aberration. “The idea is that if someone has high positive corneal spherical aberration, you would use a Tecnis. And if they had a moderate level, you would use the Alcon IQ. And then in eyes with low corneal spherical aberration, you would use a zero-aberration lens,” he said. “But here’s the real question: Is the marginal improvement in contrast sensitivity worth the trade-offs regarding diminished depth of field and tolerance to residual defocus?”
Dr. Pepose pointed to a large, contralateral-eye Swedish study that compared the zero-impact Akreos Adapt aspheric lens by Bausch + Lomb with AMO’s negatively aspheric Tecnis IOL in 80 patients. Tecnis eyes had lower totals of higher-order aberrations, and Akreos eyes had greater depth of field. But acuity and contrast sensitivity did not differ statistically. Asked about visual quality, 28 percent of subjects judged it as better in the Akreos eye, while 14 percent picked the Tecnis eye—and 58 percent had no preference.9 “My interpretation of that is that people might appreciate a little more depth of field, but I’m not sure the average patient will notice the difference in contrast sensitivity,” Dr. Pepose said.
Either go for perfection or forget it. So, for nearly all of his cataract patients who have not had refractive surgery, Dr. Pepose neither adds nor subtracts spherical aberration. He uses a zero-aberration IOL. Preserving corneal spherical aberration has the added advantage of making the eyes more tolerant of defocus, he said. “Without spherical aberration, the quality of vision drops off much faster if you don’t hit your refractive target exactly. While the image quality with the negative spherical aberration lens is superior to the zero-aberration IOL, at a plano outcome the patient’s vision with 0.5 D of defocus would be worse with the negative spherical aberration lens than it would with the zero-aberration lens. In other words, if you eliminate all of the eye’s spherical aberration, it works well if you hit emmetropia exactly, but there is less tolerance and more impact on image quality if you don’t.”
Conquer Zernike’s lower orders first. Indeed, whichever aspheric IOL is chosen, the surgeon’s accuracy in hitting the refractive target is one of the most important determinants of refractive success, Drs. Devgan and Pepose both said. They recommend using a toric IOL for astigmatism greater than 1.5 D, and correcting lower levels with limbal relaxing incisions or by making the phaco incision along the steep meridian.
“Of the whole refractive prescription of the eye, the lower-order aberrations—myopia, hyperopia and astigmatism—are 90 percent of the equation,” Dr. Devgan said. “It is more important to nail the lower-order aberrations than it is to go after higher-order branches on the Zernike tree. I’d rather have a patient with no residual astigmatism than one who has no spherical and other higher-order aberrations.”
___________________________
1 Wang, L. and D. D. Koch. J Cataract Refract Surg 2007;33:1713–1720.
2 Artal, P. et al. J Opt Soc Am A 1993;10(7):1656–1662.
3 Guirao, A. et al. Invest Ophthalmol Vis Sci 1999;40(1):203–213.
4 Holladay, J. T. et al. J Refract Surg 2002;18(6):683–691.
5 Packer, M. et al. J Cataract Refract Surg 2004;30(5):986–992.
6 Denoyer, A. et al. J Cataract Refract Surg 2009;35(3):496–503.
7 Marcos, S. et al. J Refract Surg 2005;21(3):223–235.
8 Altmann, G. E. et al. J Cataract Refract Surg 2005;31:574–585.
9 Johansson, B. et al. J Cataract Refract Surg 2007;33(9):1565–1572.
___________________________
Dr. Devgan is a consultant to Abbott Medical Optics, Bausch + Lomb and Hoya Surgical Optics, and is a stockholder in, and has received travel support from, Alcon Laboratories. Dr. Pepose is a consultant for Abbott Medical Optics, Bausch + Lomb and Acufocus, and is on the scientific advisory board for Calhoun Vision.